CABG vs. PCI in high-risk multivessel disease (Diabetics or low LV function)
Contents
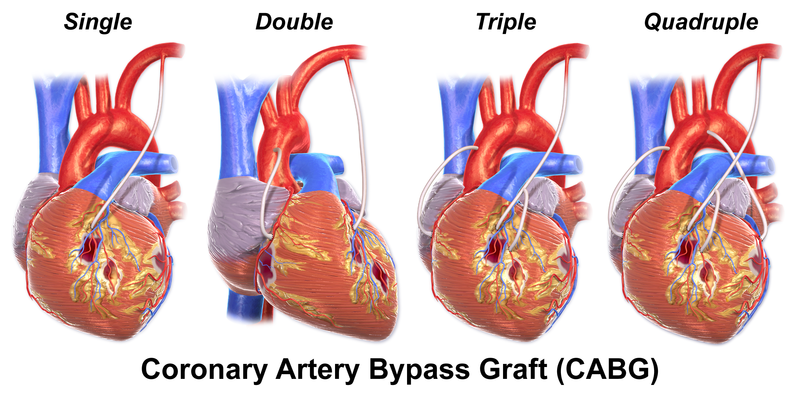
CAD in diabetics has been shown to be more aggressive and to be associated with an impaired event-free survival after both CABG and PCI because of smaller vessel sizes, longer lesion length, greater plaque burden, and a possibly differently acting restenotic cascade than in non-diabetics [5, 6]. Given this higher-risk profile, which is most often associated with multivessel disease, CABG has been regarded by some as a preferred revascularization method because of its ability to bypass this large amount of plaque burden and to achieve more complete revascularization rates, making the need for repeat revascularizations less likely.
Many trials have demonstrated CABG to be superior compared to PCI in high-risk patient subgroup. A propensity analysis [7] of long-term survival after surgical or percutaneous revascularization in 6033 patients with MVD and high-risk features (diabetes or left ventricular dysfunction) showed that PCI had 2.3 times higher mortality rate than CABG at five-year follow-up [7]. Niles et al. [8] published the results of survival of patients with diabetes and MVD after surgical or percutaneous coronary revascularization [8]. Their results showed that in 2766 risk matched diabetics PCI increased five-year mortality by 1.5–3.9 times. In a retrospective cohort study of 6320 procedures, Pell et al. compared the survival following CABG vs. PCI in diabetic and non-diabetic patients [9]. Results showed that PCI had 3.6 times higher mortality rates at two-year follow-up in patients with diabetes. New York registry of 37,212 CABG and 22,102 PCI patients with >2VD showed that after three years, CABG significantly reduced the risk of death. If the patients had >2VD and proximal LAD surgery, patients were 35% more likely than the others to be alive after three years [10]. If the patients had >2VD but no proximal LAD lesion then surgery patients were 24% more likely than the others to be alive after three years. Van Domburgh et al. reported the results of a single-center matched–propensity controlled cohort study which revealed the late outcome after stenting or CABG for treatment of multivessel disease [11]. In this matched cohort study with an 8-year follow-up, survival was better and less repeat revascularizations were needed among patients undergoing elective CABG for the treatment of multivessel disease as compared with the stent group.
In a recent study of patients with multivesel disease and ≥5 years of follow-up, CABG was found to have a significant survival advantage over patients undergoing stent implantation [12]. This advantage was maintained among most subgroups, including males, those >65 years of age, patients without a history of PCI, CABG, or MI, non-diabetics, diabetics, patients with an EF >40%, patients with either 2- or 3-vessel disease, and for both complete and incomplete PCI. The only subgroups in which the survival advantage trended toward stent implantation were those with a previous history of coronary revascularization (either previous CABG or PCI). CABG patients also experienced fewer repeat revascularizations (CABG or PCI) and MI, and 41% fewer events for the composite end point of MACE. These results are consistent with the reports of other observational studies [11, 13]. However, at one year, as in the SOS trial, there was no significant difference in the outcome of mortality [14].
However, it should be noted that most of the prior trials of CABG vs. PCI included outdated technology and techniques for both procedures – this is often why trials such as BARI [15] are no longer given the same weight.
Most of the randomized clinical trials report similar 5-year mortality rates for both CABG and PCI [1–4, 11–28]. Why the results differ between the observational studies of patients seen in typical clinical practice and these randomized trials has been addressed before (such as randomized trials eliminate selection bias, and involve independent data safety monitoring board, core laboratories and clinical event committees; registry data can be complementary in that a broader cross-section of patients are enrolled, but are subject to selection bias and inability to adjust for unmeasured confounders). Patient selection could possibly explain the differing results. Typically, clinical trial participants are required to meet strict inclusion and exclusion criteria. They often have less comorbidity and may not represent the average patient presenting for a coronary intervention. Another possible explanation for the non-significant difference in mortality between the treatments may be limited to insufficient power of these trials. Nonetheless, the SOS trial found lower mortality rates during long-term follow-up among patients randomized to CABG compared with PCI (with stents) [14]. Other randomized trials, such as the BARI study, also have found a survival advantage for CABG among certain subgroups of patients such as diabetics [21].
In this regard, two of the largest trials of CABG vs. PCI ever performed, FREEDOM (Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease) and SYNTAX trials [30] (The Synergy between PCI with TAXUS and Cardiac Surgery), both using drug-eluting stents (DES) and minimally invasive surgery have been initiated.
Recently, presented SYNTAX Trial [30] (The Synergy between PCI with TAXUS and Cardiac Surgery) results showed that PCI with TAXUS (paclitaxel-eluting) stenting was inferior to CABG with respect to the primary composite of death, stroke, MI, or repeat revascularization among patients with left main and/or 3VD. The trial was conducted at 62 sites in Europe and 23 sites in the US and had an ‘all-comers’ design instead of a highly selected population to reflect, as much as possible, real world conditions. Limited exclusion criteria included previous interventions, acute MI with creatine phosphokinase (CPK) – myocardial band >2X or concomitant cardiac surgery. Investigators randomized 1800 subjects to CABGC (n=897) or PCI (n=903). Approximately 28% had diabetes, 33% prior MI, and 29% recent unstable angina. The average number of lesions was 4.4 with 66% qualifying on the basis of three-vessel disease only, 3% with left main only, and 31% with both left main and three-vessel disease. Average stent implantation per patient was 4.6 with 48% receiving >5 stents. The primary end point of the trial, the rate of MACCE (Major Cardiovascular or Cerebrovascular Event Rate) as defined by all-cause death, cerebrovascular accident, documented MI, or any repeated revascularization at 12 months, occurred in more patients undergoing PCI than CABG (18% vs. 12%; P=0.0015). Among the subgroups presented, patients with diabetes, isolated three-vessel CAD, and left main plus involvement of an additional two or three vessels tend to have better outcomes with CABG, while outcomes in patients with isolated left main disease and left main plus a single additional vessel tended to favor PCI. One interesting observation in this study is that; although 91% had three-vessel diseases, only 4% had heart failure. Even though the study did not exclude the patients with low EF, the average mean EF was higher than 40% [28]. Hence, one might think that the outcomes might have favored CABG more if a high number of patients with LV dysfunction were enrolled.
In summary, CABG remains the first-line therapy in patients with high-risk multivessel disease with diabetes and LV dysfunction.

Comments 2
Pingback: The MASS II Study - Cardiac Health
Pingback: Optimal Medical Therapy with or without PCI for Stable Coronary Disease - Cardiac Health