Stents will last forever if they are made of some sort of metal as most are. There is a new product on the market, a new heart stent that dissolves in the artery three years after being implanted. It is yet to be used in clinically, and it will be a while (years) before its risks & benefits will be known.
(From: Scrutiny of Stent Problems Turns to Doctors, WSJ, May 29, 2007)
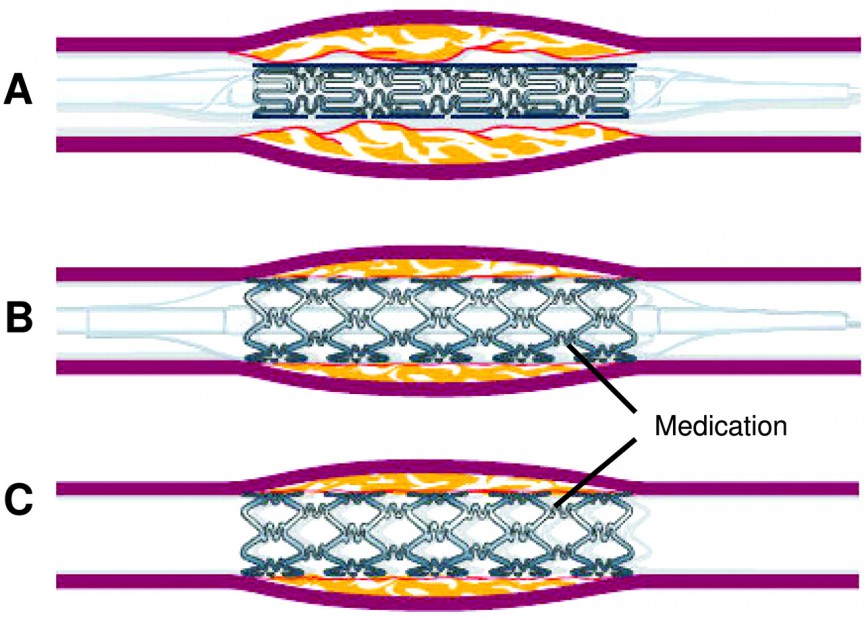
Therefore the question is not about stent durability, but about keeping the coronary artery opened up in the location where it was deployed. Because a stent destroys the artery locally, there will be scar tissue that rapidly grows over the stent. In addition, there is a strong tendency for clots to form at the site where the stent damages the arterial wall. Since platelets are involved in the clotting process, patients must take anti-platelet therapy afterwards, usually clopidogrel (Plavix) for six months and aspirin indefinitely.
Neither stents nor coronary artery bypass surgery treat atherosclerosis, the disease process that causes coronary artery disease with obstructive blockages. That means you may be developing new obstructions elsewhere, even after a successful intervention.
That said, there is about a 10-15% failure rate of stents to stay open and more than 40% of patients with a stent will need another procedure within a year, despite the use of expensive medications. This is in sharp contrast with a bypass operation that has a >95% success rate. While stents are more or less successful as treatment of anginal symptoms, they do not protect against future heart attacks or prolong life, again as opposed to bypass surgery:
If you have coronary artery disease, it is important to choose the right treatment that should in all cases include life style modifications (diet & exercise) and medications that include cholesterol meds (the only way presently to stop progression of atherosclerosis – a process that will take years). It has been shown that in most patients with stable symptoms, this last option, called “Optimal Medical Therapy”, is actually a better treatment option than Stenting.
Patients with extensive (“3 vessel”) disease that may include a “Left main stenosis”, diminished heart function and/or Diabetes do much better with a bypass operation. In situations where time is of the essence, such as an acute heart attack, a stent is may the best option if treatment is quickly enough. The same is probably also true for patients with only “one or two” vessel disease, although there are mini bypass operations that offer an equal if not superior treatment because it promises a much better long term protection.
The following includes an article from HealthDay News in 2012:
Many people with stable heart disease undergo an expensive artery-opening procedure when medication would work just as well, a new study suggests. The procedure involves placing a tiny mesh stent, or tube, in a clogged artery. As many as three-quarters of these operations are unnecessary, said lead researcher Dr. David L. Brown, a professor of medicine at Stony Brook University Medical Center in New York.
Money is the driving force, Brown said. “Everybody gets paid to put in stents, the hospital gets paid, the doctor gets paid, the stenting company gets paid,” he said. “It’s how our fee-for-service environment has taken over the decision making of this branch of cardiology.” Stenting costs an average of $9,500 more to the patient over a lifetime compared with medication, Brown said. Although the procedure, called percutaneous coronary intervention, reduces death and future heart attacks for someone actually having a heart attack, its use in stable heart disease patients is questionable, he noted.
For the study, published Feb. 27 in the Archives of Internal Medicine, Brown and Dr. Kathleen Stergiopoulos, an associate professor of clinical medicine at Stony Brook, analyzed eight trials involving more than 7,000 patients randomly assigned to medical therapy or stenting plus medication. The trials were begun between 1997 and 2005. In this type of study, called a meta-analysis, researchers look for patterns that might not have been the main intent of the individual trials.
During an average follow-up of more than four years, no significant differences were seen in longevity or quality of life.
Overall, 649 patients died, 322 who received stents and 327 who received medication alone, the study found. Nonfatal heart attacks were suffered by 323 patients with stents and 291 taking only medication.
Among those with stents, 774 needed new procedures to open blocked heart arteries. Among those on medical therapy, 1,049 also needed a procedure to open blocked arteries.
Of more than 4,000 patients for whom data on chest pain — called angina — was available, 29 percent of those with stents had persistent chest pain compared with 33 percent of those on medical therapy alone, Brown found.
There is no data that stenting patients with stable heart disease reduces the risk of dying or having a heart attack, Brown said.
“This is not to say no one will need stenting, but only about a third of patients treated initially with medical therapy will need to cross over to stenting,” he said. “People shouldn’t blindly agree to have procedures unless the doctor can tell them that there is a documented benefit” in quality or length of life, he said.
Quality of life involves relief of chest pains, he said. If patients on the best medication still have chest pain that is unacceptable to them, stenting becomes appropriate, Brown said. Medical therapy included aspirin to prevent clotting, beta blockers and ACE inhibitors or angiotensin receptor blockers to control blood pressure, and statins to lower cholesterol, the researchers noted.
“If you go the medical therapy route, it means the patient has to be followed in an outpatient environment to see how they are responding to the medical therapy, and that takes time and effort that doesn’t reimburse very well,” he said. “That’s part of the equation that drives putting in a stent rather than following the patient on medical therapy.”
Dr. James Blankenship, a spokesman for the Society for Cardiovascular Angiography and Interventions, wasn’t surprised by the study. “This is largely old news and many interventional cardiologists are avoiding the pitfalls that the authors are pointing out,” he said. “In fact, the volume of interventions among Medicare patients has gone down 18 percent between 2005 and 2010.”
“For many people, conservative medical therapy is the right thing, but for those who have a lot of symptoms, having a coronary intervention is a reasonable strategy,” he said.
Dr. Gregg C. Fonarow, co-director of the University of California, Los Angeles Preventive Cardiology Program at the David Geffen School of Medicine, agreed that medical therapy is the first choice for patients with stable heart disease.
Coronary stenting should be reserved for those patients who have worsening symptoms despite optimal medical therapy, he said.
For patients with stable coronary artery disease, “the most effective and valuable therapy to prevent disease progression, heart attacks, stroke, heart failure and premature cardiovascular death is a combination of medications together with lifestyle modification,” Fonarow added.
See the live video session that I recorded on 4/25/2014 to discuss stenting in detail!