Conclusion
Contents
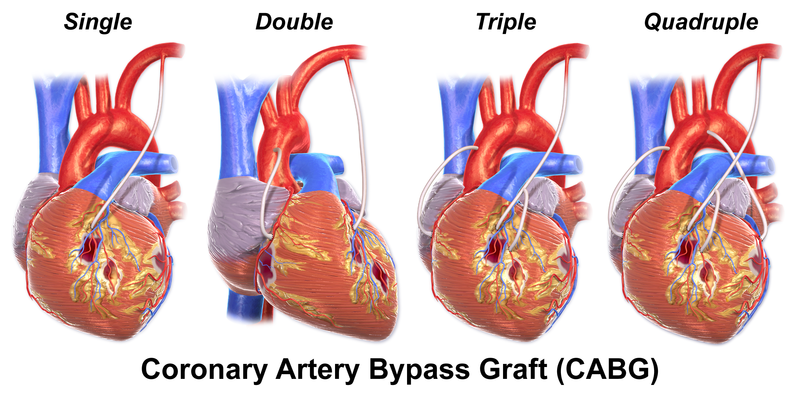
In determining a treatment strategy for a patient with CAD, there are a variety of considerations that need to be made when selecting the appropriate treatment to prevent iatrogenic fulminans [46]. Since the clinical outcomes differ according to the treatment choice as demonstrated above, it is important to replace ‘multivessel disease’ terminology with the number of diseased vessel; such as 2VD or 3VD.
FREEDOM trial is now underway, which may address many of the limitations of previous studies, and be more relevant to contemporary practice. Until then, currently available data emphasize the fact that CABG remains an excellent and often superior long-term form of revascularization in some selected groups of patients with two-vessel diseases and most groups of patients with three-vessels CAD.
It is extremely important to establish a multidisciplinary team of general cardiologists, interventional cardiologists and cardiothoracic surgeons to ensure that the most appropriate advice is offered including recommendation for stenting. Steps should be undertaken to increase the representation of cardiothoracic surgeons in the various Guidelines Writing Committee Task Force on the use of PCI vs. CABG in management of CAD (Fig. 1) to represent an unbiased opinion.
Figure 1

Fig. 1. Number of Cardiologists vs. Surgeons in the Guideline Committees and Recommendations for PCI. ESC, European Society of Cardiology; ACC, American College of Cardiology; AHA, American Heart Association; BCS, British Cardiac Society.

Comments 2
Pingback: The MASS II Study - Cardiac Health
Pingback: Optimal Medical Therapy with or without PCI for Stable Coronary Disease - Cardiac Health