In March 2013, I participated in a Podcast and several articles, published as “New fronts in heart disease: perspectives from a heart surgeon” in the Digital Journal. In it, I had the opportunity to discuss advances in the the treatment and prevention of heart disease. These were the questions that I addressed during the interview. For the answers I chose from a large variety of topics, outlined below. Of course, this is a very incomplete list, but nonetheless it involved far more that what could be covered in a half-hour podcast:
Diagnosis
- EMT
- The ability of ambulance personnel to perform EKGs, diagnose heart attacks at the scene and start treatment on anyone at risk for having a heart attack has resulted in a dramatic change in how quickly patients can get to the cath lab and get treated if necessary especially in the treatment of Acute Coronary Syndrome.
- CTCA
- MRI scans
Treatment & Prevention
- Reduction of risk factors
- Diet & Exercise
- Cardiology
- New generation stents
- Ablation
- Acute coronary syndromes (ACS)
- Optimal treatment for patients with acute myocardial infarction with ST-segment elevation (STEMI) includes early reperfusion with primary percutaneous coronary intervention (PCI) or thrombolytic therapy. However, approximately one third of eligible patients do not receive early reperfusion therapy, in many cases because of late presentation.
- Don’t perform stenting of non-culprit lesions during percutaneous coronary intervention (PCI) for uncomplicated hemodynamically stable ST-segment elevation myocardial infarction (STEMI).
- Optimal treatment for patients with acute myocardial infarction with ST-segment elevation (STEMI) includes early reperfusion with primary percutaneous coronary intervention (PCI) or thrombolytic therapy. However, approximately one third of eligible patients do not receive early reperfusion therapy, in many cases because of late presentation.
- CAD in women
- Advanced Heart Disease/Heart Failure
- ICD and Resynchronization therapy
- Arrhythmias
- Medications
- Hypertension
- Renal artery denervation
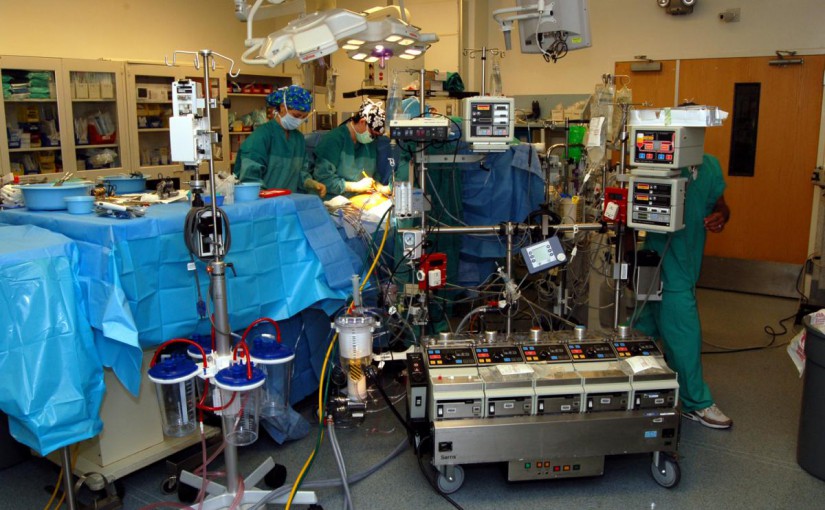
- Cardiac Surgery
- Minimally invasive heart surgery, OpCAB, MidCab, Robotic surgery
- Valve repair
- TAVI
- TEVAR (thoracic endovascular aortic repair)
II. With any innovation, there often emerges an equation between innovation and cost-effectiveness. With the Affordable Care Act and other cost-saving pressures being applied over the coming years, how will these innovations continue to improve cardiovascular care?
In the treatment of CAD many studies have shown Optimal Medical Therapy is more effective for patients with stable Coronary Artery Disease, at a fraction of the cost. Interventions should be limited to those at risk (85% of PCI may not be indicated):
In a January 4th, 2012 JAMA editorial, the authors describe that patients were not being helped by a variety of well-established procedures including stenting for stable coronary artery disease:
“Percutaneous coronary intervention (stenting) performed for stable coronary artery disease… cost(s) billions of dollars and (has supported) the existence of (an) entire specialty for many years. Stable coronary artery disease accounted for 85% of all stenting in the United States at the time of the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial. Large, well-designed randomized trials that tested whether these practices improved major patient outcomes revealed that patients were not being helped. Defenders of these therapies and interventions wrote rebuttals and editorials and fought for their specialties, but the reality was that the best that could be done was to abandon ship... There are thousands of clinical trials, but most deal with trivialities or efforts to buttress the sales of specific products. Given this conundrum, it is possible that some entire medical subspecialties are based on little evidence.
The results of COURAGE have done little to improve optimal medical management of stable coronary artery disease prior to invasive intervention. Stenting may not improve mortality, but the procedure apparently diminishes angina.
CABG remains the standard of care and is by far the more cost-effective in comparison with stents (w/i one year!).“
The editorial is consistient a number of articles we have written for this website, including reviews of the SYNTAX trial and in a letter to to the editor of Wallstreet Journal in 2010.
Patients with stable coronary artery disease (85% of all patients who undergo stenting in the US!) are recommended procedures that will not prolong their lives, nor prevent recurrences and thus
- Face repeat stenting at regular intervals,
- Face discontinuation of (very expensive) medications at their peril.
III. Heart surgery appears to be increasingly about the implementation of technology (valve replacements and stent treatments). What are the technologies making the difference? Where do you see technology playing a bigger role?
- Off – On Pump CABG, minimally invasive CABG
- Robotic Surgery
- TAVI
- Thoracic Aortic Aneurysm, dissection and Traumatic aortic injuries
- TEVAR
- Surgery for Heart Failure:
- Heart transplantation
- Artificial heart
IV. CardiacHealth.org shares content on diet and exercise with a mind toward preventative measures. With regard to heart disease prevention, where are you seeing the most success? Where can there be better improvements?
- Prevention
- Obesity
- Metabolic syndrome. The chance of developing metabolic syndrome is closely linked to obesity and a lack of physical activity.
- Diet
- Exercise
V. As the population ages and longevity is now a very real issue, what do these demographic changes mean for heart surgeons and for cardiovascular care in general?
Heart surgeons have seen a reduction of >30% in case volume. Both CABG and PCI are mature well established procedures for the treatment of CAD. However, despite 2012 AHA Standard of Care Recommendations that include CABG for patients with 3V CAD and L main disease, especially in diabetics and those with reduced cardiac function, the standard of Practice remains PCI:

Comparison of stenting with CABG
The facts:
Among patients with stable coronary artery disease, percutaneous coronary intervention (PCI) exhibited no significant effect in reducing the risk of death, myocardial infarction, or other major cardiovascular events.
Adding PCI to optimal medical therapy (OMT) was not proven a cost effective initial management strategy for symptomatic chronic coronary artery disease.
BEFORE publication last month of the SYNTAX AND FREEDOM trials, the general consensus was that stenting offered the same survival benefits as open-heart bypass surgery, NOT TRUE.
SYNTAX AND FREEDOM suggest otherwise:
CABG results in half the death rate and one- third the heart attack rate of PCI some five years after either procedure has been carried out.
After five years, surgery was found to have limited major adverse cardiac and cerebrovascular events to 27 per cent of participants in the CABG group compared with a complication rate of 37.3 per cent in the PCI group.
While almost 10 per cent of those who underwent a stenting procedure had had a heart attack at follow-up, just fewer than 4 per cent of those who had a CABG suffered a heart attack.
Deaths from a cardiac cause were at 5 per cent of those who went down the bypass route, compared with 9 per cent of participants who had a stent inserted.
And when it came to the need for a repeat procedure over the five years, some 14 per cent of the CABG group required one as against 26 per cent of those who underwent a PCI.
Heart team
- Away from the figures, the researchers found those who had been looked after using a team approach did better. In other words, rather than cardiac surgeons and cardiologists working in isolation, being treated by a “heart team” – consisting of a core minimum of an interventional cardiologist and cardiac surgeon, and recruiting additional expertise as necessary – produced the best outcomes.
- Older patients, in general, pose a greater surgical risk while those with diabetes tend to have different patterns of heart disease compared with the rest of the population.
- What is not in doubt is that having a stent inserted is the treatment of choice for someone who develops chest pain out of the blue and is found to have an acute coronary blockage.
- But this latest research is a game-changer for people diagnosed with stable coronary artery disease.
- Depending on the exact location and number of blockages in the coronary system, bypass surgery may well be a better long-term option.
- The most important point to emerge from this research for anyone faced with coronary artery disease is to ask for their case to be discussed at a multidisciplinary meeting at which both a cardiac surgeon and cardiologist are present.