- Thoracic Aortic Aneurysms
- Symptoms of Thoracic Aortic Aneurysms
- Causes of Thoracic Aortic Aneurysms
- Aortic dissection
- Traumatic Aortic injury
- Diagnosis
- Treatment
- Surgical repair
- Endovascular repair
Thoracic Aortic Aneurysms
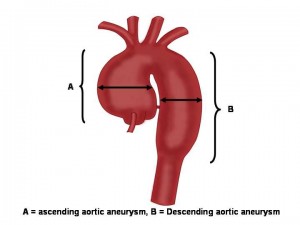
An aneurysm that occurs in the part of the aorta that’s located in the chest and above the diaphragm is called a thoracic aortic aneurysm. TAAs account for 1 in 4 aortic aneurysms. Ascending aortic aneurysms are the second most common aortic aneurysm to abdominal aortic aneurysms. Most ascending aortic aneurysms are diagnosed in patients in their sixth and seventh decade of life.
TAAs don’t always cause symptoms, even when they’re large. Only half of all people who have TAAs notice any symptoms. TAAs are found more often now than in the past because of chest CT scans done for other medical problems.
With a common type of TAA, the walls of the aorta weaken, and a section close to the heart enlarges. As a result, the valve between the heart and the aorta can’t close properly. This allows blood to leak back into the heart.
A less common type of TAA can develop in the upper back, away from the heart. A TAA in this location may result from an injury to the chest, such as from a car crash.
When an artery wall in the aorta weakens, the wall abnormally expands or bulges as blood is pumped through it, causing an aortic aneurysm. The bulge or ballooning may be defined as a:
- Fusiform: Uniform in shape, appearing equally along an extended section and edges of the aorta.
- Saccular aneurysm: Small, lop-sided blister on one side of the aorta that forms in a weakened area of the aorta wall.
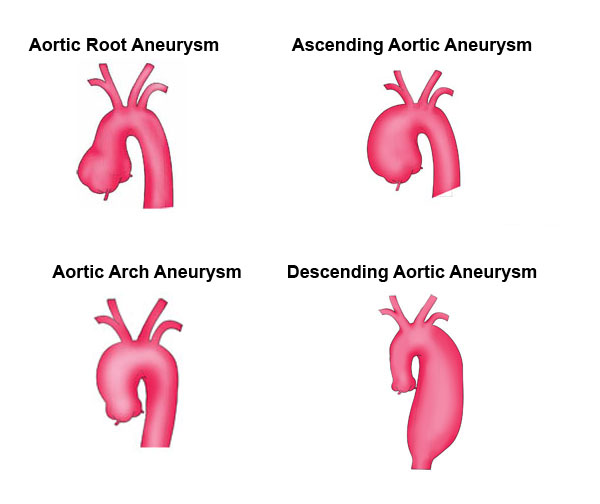
An aneurysm can develop anywhere along the aorta:
- Aneurysms that occur in the section of the aorta that runs through the abdomen (abdominal aorta) are called abdominal aortic aneurysms.
- Aortic aneurysms that occur in the chest area are called thoracic aortic aneurysms and can involve the aortic root, ascending aorta, aortic arch or descending aorta.
- Aneurysms that involve the aorta as it flows thru both the abdomen and chest are called thoracoabdominal aortic aneurysms.
Thoracic aortic aneurysms affect approximately 15,000 people in the United States each year.
A thoracic aortic aneurysm is a serious health risk because, depending on its location and size, it may rupture or dissect (tear), causing life-threatening internal bleeding. When detected in time, a thoracic aortic aneurysm can often be repaired with surgery or other less invasive techniques.
Small aneurysms place one at increased risk for:
- Atherosclerotic plaque (fat and calcium deposits) formation at the site of the aneurysm
- A clot (thrombus) may form at the site and dislodge, increasing the chance of strokeIncrease in the aneurysm size, causing it to press on other organs, causing pain
- Aortic dissection, or tearing of the layers of the aorta, a potentially fatal complication and a medical emergency.
- Aneurysm rupture, because the artery wall thins at this spot, it is fragile and may burst under stress. A sudden rupture of an aortic aneurysm may be life threatening and is a medical emergency
Symptoms of a thoracic aortic aneurysm
Thoracic aortic aneurysms often go unnoticed because patients rarely feel any symptoms. While only half of those with thoracic aortic aneurysms complain of symptoms, possible warning signs include:
- Pain in the jaw, neck, and upper back
- Chest or back pain
- Coughing, hoarseness, or difficulty breathing
Causes of a thoracic aortic aneurysm
Thoracic aortic aneurysms are most often caused by atherosclerosis, a hardening of the arteries that damages the artery’s walls. While your arteries are normally smooth on the inside, as you age they can develop atherosclerosis. When atherosclerosis occurs, a sticky substance called plaque builds up in the walls of the arteries. Over time, excess plaque causes the aorta to stiffen and weaken.
Your risk for atherosclerosis increases if you:
- Are a smoker
- Have high blood pressure
- Have cholesterol
- Are obesity
- Have a family history of cardiovascular or peripheral vascular disease (a narrowing of the blood vessels)
Certain diseases can also weaken the layers of the aortic wall and increase the risk of thoracic aortic aneurysms, including:
- Marfan syndrome
- Other non-specific connective tissue disorders (characterized by a family history of aneurysms)
- Presence of a bicuspid aortic valve
- Syphilis
- Tuberculosis
Rarely, trauma, such as a severe fall or car accident can cause a thoracic aortic aneurysm.
As you age, your risk of developing a thoracic aortic aneurysm increases. More men than women are diagnosed with thoracic aortic aneurysms, and are often affected with the condition at a younger age.
Recent research indicates that a substantial amount of aneurysms have familial patterns, or are inherited from previous generations. It is important to tell your physician if there is a history of aortic aneurysms in your family to ensure that the best preventative screenings are completed.
Aortic dissection
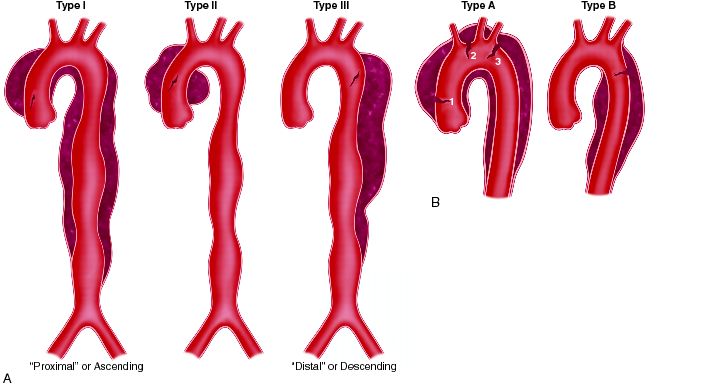
DeBakey (A) and Stanford (B) classification of thoracic aortic dissection (From: Diseases of the aorta, Cleveland Clinic)
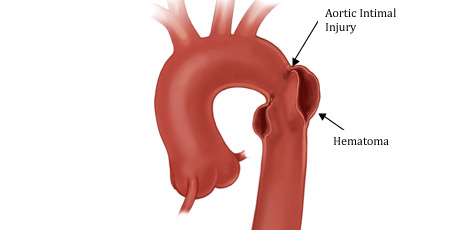
Aortic dissection occurs when the layers of the aorta tear and separate from each other. The presence of an aortic aneurysm increases your risk of having an aortic dissection, but aortic dissection can also occur in people with a normal sized aorta.
Aortic dissection can occur suddenly, causing severe sharp, tearing pain in your chest or upper back. Yet, like all types of aneurysms, there may be no symptoms of an aortic dissection.
Most commonly associated with high blood pressure, an aortic dissection forces the layers of the wall of the aorta apart through increased blood flow. If not treated early, aortic dissection weakens the aorta and can lead to a thoracic aortic aneurysm by causing the weakened area of the aorta to bulge like a balloon, stretching the aorta.
If you do experience any symptoms of a thoracic aortic aneurysm or aortic dissection, notify your physician immediately. If left untreated, these conditions could lead to a fatal rupture.
Traumatic Aortic injury or blunt Aortic injury (rupture or tear)
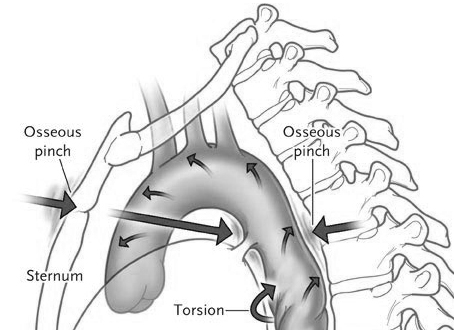
Up to 15% of all deaths following motor vehicle collisions are due to injury to the thoracic aorta. Many of these patients are dead at scene from complete aortic transection. Patients who survive to the emergency department usually have small tears or partial-thickness tears of the aortic wall with pseudoaneurysm formation.
Most blunt aortic injuries occur in the proximal thoracic aorta, although any portion of the aorta is at risk. The proximal descending aorta, where the relatively mobile aortic arch can move against the fixed descending aorta (ligamentum arteriosum), is at greatest risk from the shearing forces of sudden deceleration. Thus the aorta is a greatest risk in frontal or side impacts, and falls from heights.
Most blunt aortic injuries surviving to hospital are partial-transections, and should be managed with blood pressure control until the defintivie repair.
Diagnosis of a thoracic aortic aneurysm
Early diagnosis of a thoracic aneurysm is critical to managing the condition. The larger the thoracic aortic aneurysm, or the faster it grows, the more likely it is to rupture. The risk of rupture increases when the aneurysm is larger than about twice the normal diameter of a healthy aorta blood vessel.
Diagnosing a thoracic aneurysm is difficult because often there are no symptoms, and often the condition goes undiagnosed until a rupture occurs. If a thoracic aortic aneurysm is suspected, your physician may order the following tests:
- Chest x-ray
- Computed tomography (CT) scan
- Magnetic resonance imaging (MRI)
- Echocardiography (an ultrasound of the heart)
- Abdominal ultrasound (to look for associated abdominal aneurysms)
- Angiography (an x-ray of the blood vessels)
Treatment of a thoracic aortic aneurysm
Treatment for an aneurysm depends on its size, location and your overall health.
If the thoracic aortic aneurysm is small and not causing any symptoms, your physician may recommend “watchful waiting.” By closely monitoring your condition with CT or MRI scans every 6-12 months, the aneurysm will be watched for signs of changes.
If you have high blood pressure, your physician will prescribe blood pressure medication to lower your overall blood pressure and the pressure on the weakened area of the aneurysm. Additionally your physician may prescribe a “statin” (or cholesterol lowering medication) to maintain the health of your blood vessels.
Surgical Repair
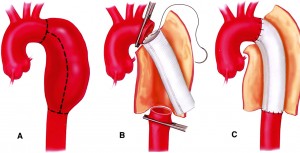
Aortic aneurysm surgically removed and replaced with a graft
If the thoracic aortic aneurysm is large or causing symptoms, you will need prompt treatment to prevent a rupture from occurring. The weakened section of the vessel can be surgically removed and replaced with a graft of artificial material. If the aneurysm is close to the aortic valve (the valve that regulates blood flow from the heart into the aorta), a valve replacement may also be recommended during the procedure.
Repairing the aneurysm surgically is complex and requires an experienced thoracic surgical team. However, neglecting the aneurysm presents a higher risk. Repairing a thoracic aneurysm may require open-chest surgery, general anesthesia and a minimum hospital stay of five days.
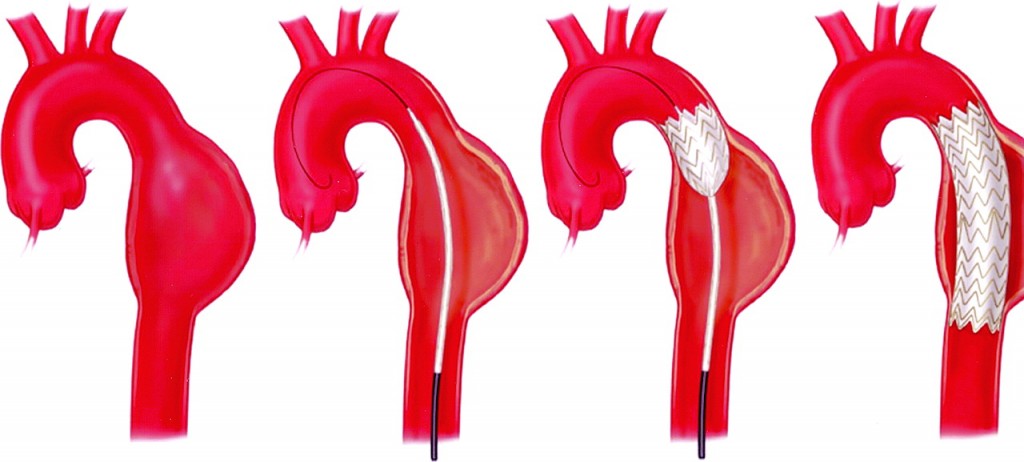
Endovascular Repair
Instead of an open aneurysm repair, your surgeon may consider a newer procedure called an endovascular aneurysm repair (EVAR, TEVAR, TA-EVAR). Endovascular means that surgery is performed inside your aorta using thin, long tubes called catheters. By entering through small incisions in the groin, the catheters are used to guide and deliver a stent-graft through the blood vessels to the site of the aneurysm. The stent graft is then positioned in the diseased segment of aorta to “reline” the aorta like a sleeve to divert blood flow away from the aneurysm.
This endovascular approach is currently used to treat abdominal and descending thoracic aneurysms, and is being evaluated as a treatment for thoracoabdominal and arch aneurysms. While current results are positive, further research is needed to determine who the best candidates for this type of procedure may be.