MASS II [i] is a small, single-center study designed to compare the long term effects of Medical Therapy (MT), Percutaneous Coronary Intervention (PCI) or Coronary Artery Bypass Grafting (CABG) among patients with stable angina, multivessel CAD and preserved ventricular function. Patients selected were appropriate candidates for all 3 therapies.
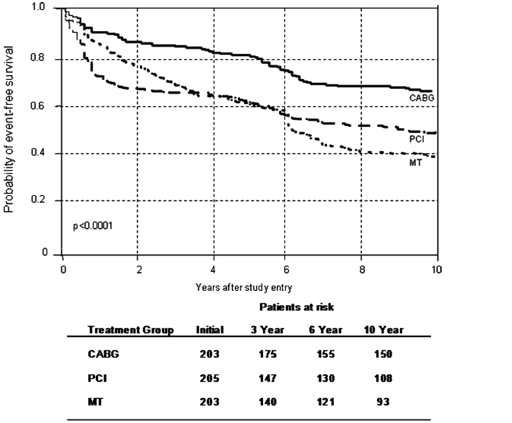
In MASS II 611 patients were randomly assigned to CABG (n=203), PCI (n=205), or MT (n=203). The 10-year survival rates were 74.9% with CABG, 75.1% with PCI, and 69% with MT (P=0.089). The trial’s primary end point was a composite of total mortality, Q-wave MI, and refractory angina requiring revascularization. Secondary end points included angina status, death due to a cardiac cause, and stroke.
At 5-year follow-up no significant differences were found between MT and PCI in the primary end points. CABG was superior than MT and PCI, although the difference in mortality was not significant.
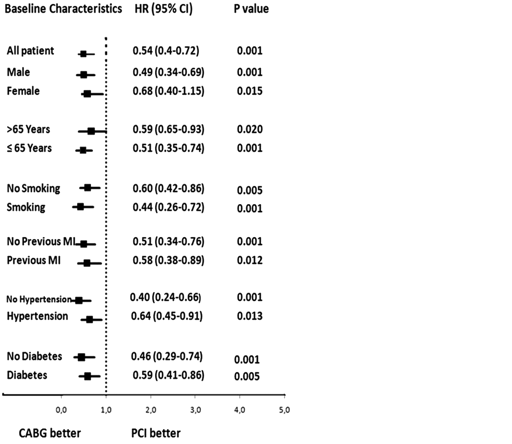
However, a significant 47% risk reduction for CABG was noted in the incidence of primary end points during 5 years of follow-up (P=0.001, 95% confidence interval [CI] 0.36 to 0.77).
Primary End points at 10 years
The 10-year rates of myocardial infarction were 10.3% with CABG, 13.3% with PCI, and 20.7% with MT (P=0.010). The 10-year rates of additional revascularizations were 7.4% with CABG, 41.9% with PCI, and 39.4% with MT (P=0.001). Relative to the composite end point, Cox regression analysis showed a higher incidence of primary events in MT than in CABG (hazard ratio 2.35, 95% confidence interval 1.78 to 3.11) and in PCI than in CABG (hazard ratio 1.85, 95% confidence interval 1.39 to 2.47). Furthermore, 10-year rates of freedom from angina were 64% with CABG, 59% with PCI, and 43% with MT (P=0.001).
At 10 years follow-up, the MASS II trial found a strong, independent, protective association between CABG and the composite primary end point compared with MT and PCI after adjustment for sex, smoking, total cholesterol, previous MI, hypertension, diabetes, and the number of diseased vessels. Additionally, MT patients had less relief from symptomatic angina than did patients who underwent CABG or PCI.
Figure 1. Probability of event-free survival (free of overall mortality, unstable angina that required revascularization, or Q-wave MI) among patients in the MT, CABG, and PCI treatment groups.
Figure 2. HRs measuring association between composite end point and treatment allocation: CABG vs PCI.
The lowest rate of repeat revascularization procedures (from the present study) was noted after CABG, whereas a substantial proportion of patients undergoing MT alone (39%) crossed over to revascularization, and 41.9% of PCI patients required repeat revascularization procedures.
Conclusion:
The 10-year results of MASS-II indicate that revascularization with CABG, improves the outcomes of patients with multivessel disease in comparison to MT and PCI in important events such cardiac death and MI, as well as subsequent revascularization procedures.