Introduction
Normal Skin
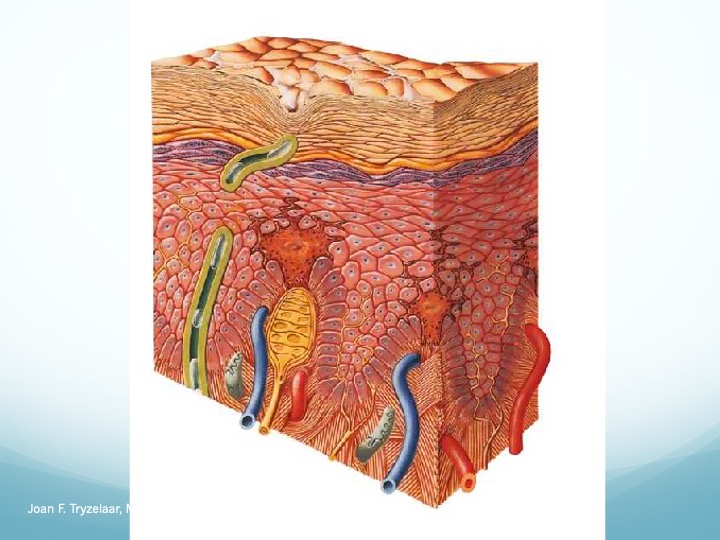
Normal healthy skin has several distinct functions. It protects underlying tissues from abrasions, entry of microbes, unwanted water loss, and ultraviolet light damage. Tactile sensations of touch, pressure, and vibration; thermal sensations of heat and cold; and pain sensations all originate in the skin’s nervous system. The body’s thermoregulation relies on the skin’s ability to sweat and control blood flow to the skin to increase or decrease heat loss. The skin’s functions are performed by three distinct tissue layers: a thin outer layer of cells called the epidermis, a thicker middle layer of connective tissue called the dermis, and an inner,
subcutaneous layer. The outer layers of the epidermis are composed of flattened, cornified, dead keratinocytes that form a barrier to water loss and microbe entry. These cells are derived from keratinocytes in the basal layer, which lies above the dermis, and are responsible for skin
reepithelization. The epidermis does not contain nerves or blood vessels and obtains water and nutrients through diffusion from the dermis. The dermis is composed mostly of collagen fibers and some elastic fibers both produced by fibroblasts and, along with water and large proteoglycan molecules, makes up the extracellular matrix (ECM). This skin layer provides mechanical strength and a substrate for water and nutrient diffusion; it contains blood vessels, nerves, sweat glands, hair follicles, and cells involved in immune function, growth, and repair.
The subcutaneous layer is composed of adipocytes that form a thick layer of adipose tissue.
Chronic Wounds
Failure of any wound to heal can be due to a lack of one or more of the main requirements of healing, including a good supply of blood, oxygen and nutrients, and a clean and infection-free environment. An important aspect in caring for wounds is to remove the causing agent, as in cases of wounds caused by weight-bearing or wounds that are under constant pressure. When wounds do not get relief from constant pressure, there can be a cumulative breakdown of the tissue.
Types of Chronic Wounds
Some of the most common types of wounds and their specific causes are as follows:
- Infectious wounds: Whether it is bacterial, fungal or viral, if the cause of the infection is not treated with the proper medication, the wound will not heal properly in the expected time.
- Ischemic wounds: Ischemia means that the wound area is not getting sufficient blood supply. Limiting the blood supply, and the oxygen and nutrients it carries, can delay the healing process or even prevent it.
- Radiation poisoning wounds: Regardless of whether the source of radiation was therapeutic (gamma rays or x-rays) or accidental (exposure to radioactive materials from nuclear plant accidents or radioactive devices that detonate), excessive exposure to ionizing radiating materials can weaken the immune system, cause damage to exposed tissue and delay the healing time of all wounds.
- Surgical wounds: Wounds caused by incisions made during surgery can progress to chronic wounds if the blood supply to the surgery area was accidentally damaged or if wound care was inadequate. Both can delay the healing time of a wound.
Ulcers (the most common type of chronic wounds)
- Arterial ulcers: These can occur from hypertension, atherosclerosis (plugging) and thrombosis (clotting), where the reduced blood supply leads to an ischemic state.
- Venous ulcers: These account for more than half of ulcer cases, especially in the lower limbs (mainly the legs) as associated with deep vein thrombosis, varicose veins and venous hypertension. Venous ulcers can lead to stasis, where the blood fails to circulate normally.
- Diabetic ulcers: These are a common complication in uncontrolled diabetes mellitus, resulting in impaired immune function, ischemia (due to poor blood circulation) and neuropathy (nerve damage), which eventually lead to breakage of skin and ulceration.
- Pressure ulcer: The constant pressure and friction resulting from body weight over a localized area for prolonged duration can lead to breakage of skin and ulceration (also known as bed sores); especially on the back and on the ankles and feet.
Signs and Symptoms of Chronic Wounds
Infectious wounds: These typically have a bad odor, pus drainage, debris (yellowish to greenish) or dead tissue, and ongoing symptoms of inflammation (fever, pain, redness, hotness and swelling).
Ischemic wounds: Usually the wound area will be pale and cold. There might also be a decrease in the hair growth and a weak pulse sensation in the area.
Radiation poisoning wounds: These can present with redness, blistering, itching, inflammation and other unspecified symptoms that include nausea, vomiting, abdominal pain and fever.
Surgical wounds: Typically occur at the site of a surgical incision, but instead of a clean appearance, the tissue around the incision appears red, hot, and swollen, which can be infected or inflamed.
Ulcers
- Arterial ulcers: Usually involve the full thickness of skin, having a punched out appearance with smooth edges and occasionally pain that subsides when the legs are lowered below the heart level. In some cases, ischemia is present (poor circulation to area).
- Venous ulcers: The skin is usually shiny and smooth with minimal to no hair. These ulcers are superficial, shallow, and irregularly shaped with pain and edema. These can sometimes be associated with infection or inflammation.
- Diabetic ulcers: These can be either of neuropathic (secondary to nerve damage) origin, where the lack of sweat makes the skin dry and easy to crack and scale, forming callus (accumulation of dead skin layers). The callused area, mostly occurring on the foot, can eventually break down and form an ulcer. Diabetic ulcers can also occur from neuropathy with ischemic origin; where the ulcer area is cool with no pulse, in addition to the other signs of ischemia described above.
- Pressure Ulcers: These present with redness that doesn’t go away when pressed upon, and includes itching, blistering, hotness, swelling and discoloration of the area.
Who Is at Risk
People with the one or more of the following are at risk for developing chronic wounds:
- Chronic medical conditions, such as diabetes, high cholesterol, severe burns, cancer or AIDS
- Vascular disease, including heart disease, hypertension, atherosclerosis, anemia, varicose veins or deep venous thrombosis
- Elderly, immobile or obese people are at a greater risk
- Unhealthy lifestyle or habits like smoking, poor diet and hygiene or lack of exercise
- Previous history of ulcers, multiple surgeries or prolonged periods of bed rest
- Weak immune system, as in patients taking corticosteroids, chemotherapy or radiotherapy
- High-risk occupations with radiation exposure or long periods of sitting
Treatment and Prevention of Chronic Wounds
The best treatment is to prevent the wound from progressing to chronic state by avoiding all the risk factors. Preventative measures include maintaining proper hygiene and wound care as instructed by the doctors, while complying with the prescribed medications. Regular inspection of wounds to track healing progress is also a primary part of the treatment plan.
In general, treating and removing the underlying cause of any chronic wound should be the primary focus of the treatment. In some cases a surgical debridement (removing any accumulated dead tissue) is needed to improve the blood flow and supply of nutrients to the wound. In other cases, applying proper wound care by changing wound dressings frequently, keeping the wound clean, applying local antibiotic, taking anti-inflammatory medications when needed and maintaining a healthy lifestyle is sufficient to prevent chronic wounds and encourage proper healing.
