The Future Revascularization Evaluation in Patients with Diabetes Mellitus: Optimal Management of Multivessel Disease (FREEDOM) study enrolled 1,900 patients over a 5-year period from 2005 through 2010.
Contemporary PCI and CABG techniques and currently recommended ancillary medical therapies were examined to determine whether CABG or PCI with drug-eluting stents are the superior approach to revascularization in patients with diabetes and multivessel coronary artery disease.
Conclusion:
CABG is superior to PCI with drug-eluting stents in patients with diabetes and advanced (predominantly three-vessel) coronary artery disease. CABG significantly reduces rates of death and myocardial infarction, but with a higher rate of stroke.
Findings
In this study the 5-year mortality rate, myocardial infarction, or stroke was 26.6% among patients treated with a PCI, versus 18.7% in the coronary artery bypass graft (CABG) group (P=0.005). These findings were true for all the risk factors examined, but especially for patients with poor heart function (LVEF <40%).
Key Points
In long-term follow-up, the rate of myocardial infarction was significantly higher in the PCI group than in the CABG group, whereas the rate of stroke was significantly higher in the CABG group. However, the higher relative risk of stroke among patients undergoing CABG was evident only early in the postprocedural period:
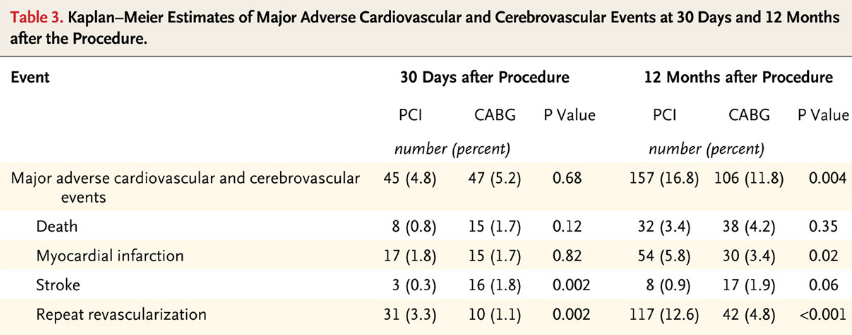
Stroke rates at 5-year were 2.4% in the PCI group and 5.2% in the CABG group. Of these strokes, the majority (87%) were ischemic and 13% were hemor- rhagic. In the first 30 days after the procedure, 3 patients in the PCI group and 16 in the CABG group had a stroke (Table 3). The excess of strokes in the CABG group occurred in the first 30 days after randomization. An NIH Stroke Scale score of more than 4 (severely disabling) at the time of the event was reported in 27% of patients in the PCI group, as compared with 55% of those in the CABG group. A score on the Rankin scale of more than 1 at the time of the stroke was re- ported in 60% of patients in the PCI group, as compared with 70% in the CABG group.
Concomitant medical therapy is important to all patients with diabetes and coronary artery disease. Unlike in SYNTAX, almost 90% of patients in both the CABG and PCI groups received dual antiplatelet therapy.
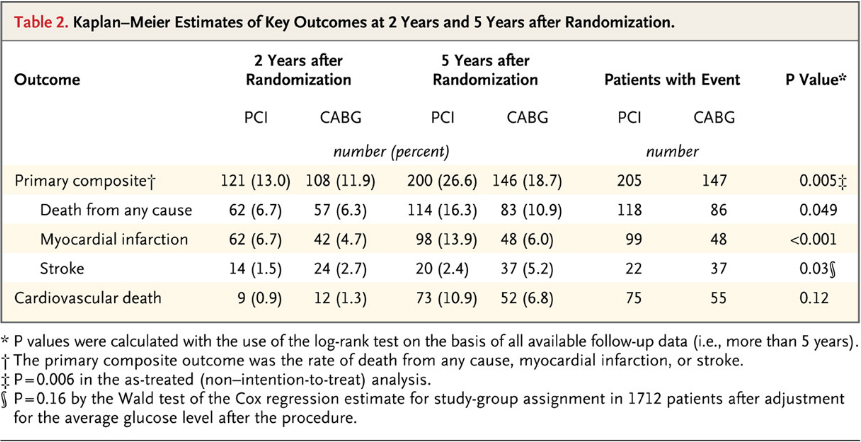
Kaplan–Meier Estimates of Key Outcomes at 2 Years and 5 Years after Randomization:
Kaplan–Meier Estimates of the Composite Primary Outcome and Death:
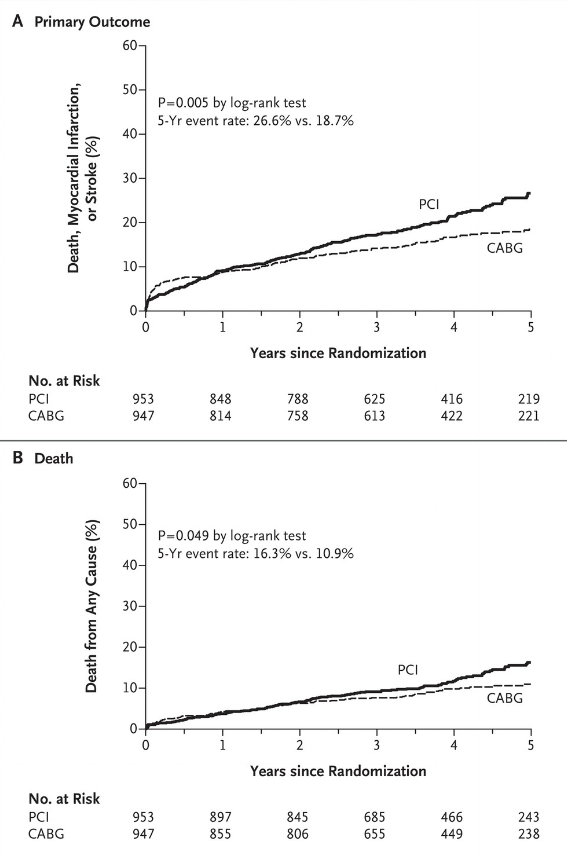
Shown are rates of the composite primary outcome of death, myocardial infarction, or stroke (Panel A) and death from any cause (Panel B) truncated at 5 years after randomization. The P value was calculated by means of the log-rank test on the basis of all available follow-up data.
Kaplan–Meier Estimates of Major Adverse Cardiovascular and Cerebrovascular Events at 30 Days and 12 Months after the Procedure:
Primary Composite Outcome, According to Subgroup:
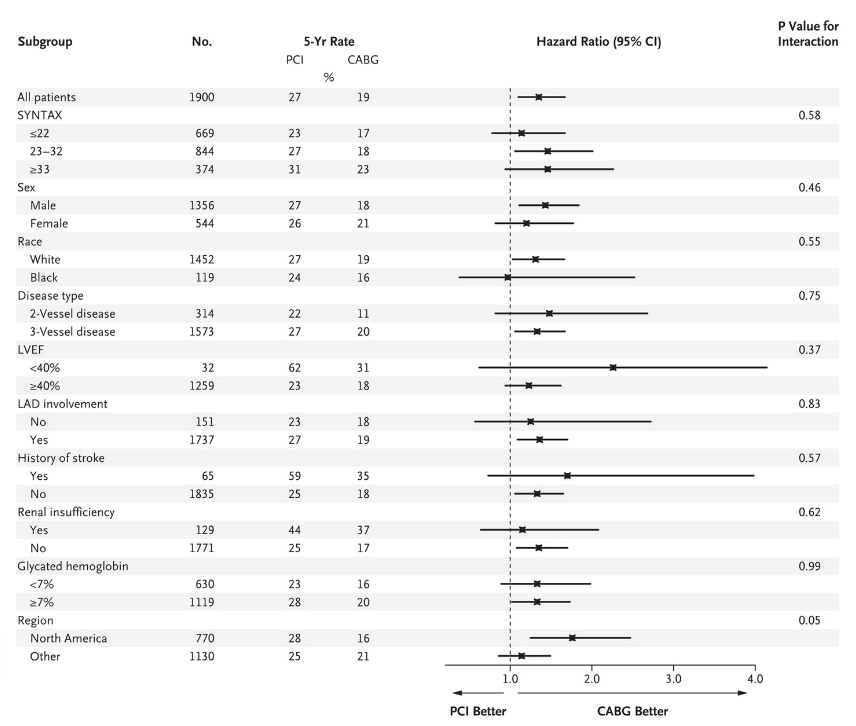
Subgroup analyses were performed with the use of Cox proportional-hazards regression. Five-year composite event rates for death, myocardial infarction, or stroke are shown. LAD denotes left anterior descending artery, and LVEF left ventricular ejection fraction.
Reference:
Farkouh, ME et al “Strategies for mulitvessel revascularization in patients with diabetes” NEJM 2012; DOI: 10.1056/NEJMoa1211585.

Comments 3
Pingback: The MASS II Study - Cardiac Health
Pingback: Cost-Effectiveness of PCI with Drug Eluting Stents versus CABG - Cardiac Health
Pingback: Optimal Medical Therapy with or without PCI for Stable Coronary Disease - Cardiac Health