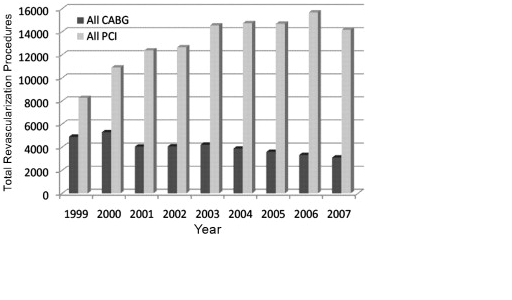
In a large comparative study, interventions for CAD were compared. From 1999-2007 more than 150000 interventions were performed in Washington State. During that period, the volume of PCI procedures increased by 71%, while simultaneously, CABG diminished by almost 40%. In final analysis, PCI was almost five times more likely to happen than CABG.
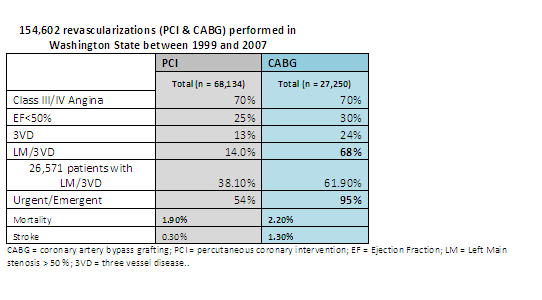
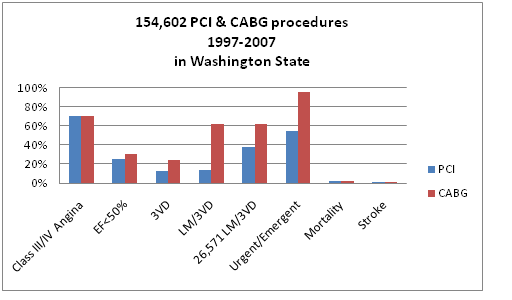
For patients undergoing CABG, the prevalence of, hypertension and three-vessel or left main disease increased significantly (p < 0.0001 for all). Despite an increasing acuity of risk factors, mortality (2.4% to 2.2%; p = 0.79) was unchanged, while the incidence of stroke improved significantly in the past 9 years.
Owing to larger numbers, temporal changes were even more significant in patients undergoing PCI with NPR, with increased acuity and severity of many known co-morbidities. There was a modest increase in age, cerebral vascular disease, DM, Canadian heart class (III and IV), and LM/3VD. Very significant and much more dramatic was an increase in PCI for acute MI. Clinical outcomes for PCI remained stable and unchanged.
- In this study, almost 2/3 of the patients diagnosed with LM/3VD underwent PCI as opposed to the widely accepted current criteria for coronary revascularization.
- The dramatic loss of CABG volume was associated with statistically significantly increases in risk profiles of CABG patients. Most importantly, these changes did not adversely impact surgical outcomes. Mortality was unchanged with decreased morbidity (stroke, MI, transfusion, ventilator time; adjusted p < 0.01 for all).
- Risk profiles of patients undergoing PCI also increased during this time interval with a dramatic rise in emergency procedures, reflecting PCI for acute MI or unstable coronary syndromes now representing 33% of all PCI procedures in patients with NPR. This practice unexpectedly resulted in the highest mortality (double) and morbidity in patients undergoing PCI with no prior revascularization.
- This data strongly suggests that current clinical seems to embrace a strategy of limited intervention of an isolated anatomic target lesion thought to be culpable for the patient’s symptoms.
- Such treatment purposely defers treatment of known residual concurrent coronary disease to future re-interventions.
- The long-term consequences of this departure from more complete revascularization strategies on mortality, cardiac morbidity, and costs are unknown, and are in conflict with the current published guidelines.
A subset of patients with diabetes and 3VD was examined in a 2nd paper from Washington State 2). The purpose of this study was to examine the application of revascularization strategy in this high-risk patient population in a real-world/clinical practice setting. Specifically, it was sought to determine: (1) the revascularization strategies employed in diabetic patients with MVD in Washington State; (2) the short-term outcomes of revascularization strategies; and (3) the effect of DES introduction has had on the revascularization strategy.
Since these studies have only described procedural and short term outcomes, it would be interesting to see if follow-up data (when available) indeed confirm trends noticed elsewhere, such as re-intervention and the absence of any survival benefit,
Dr T
From:
1) Changing Volumes, Risk Profiles, and Outcomes of Coronary Artery Bypass Grafting and Percutaneous Coronary Interventions, Gabriel S. Aldea, MD et al. Ann Thorac Surg 2009;87:1828 –38
2) Prevalence and Procedural Outcomes of Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting in Patients with Diabetes and Multivessel Coronary Artery Disease, Nahush A. Mokadam M.D. et al, J. Cardiac Surgery, 3 OCT 2010)