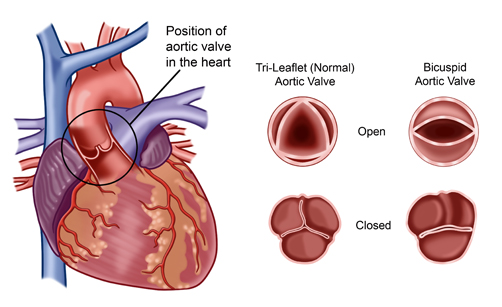
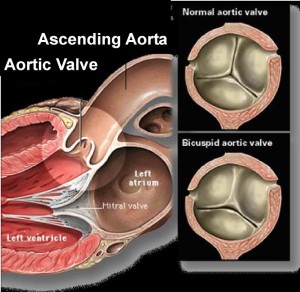
Bicuspid aortic valve disease (BAV) is a congenital condition (present at birth) and occurs in about two percent of the population. Instead of the normal three leaflets or cusps, the bicuspid aortic valve has only two.
Without the third leaflet, the valve may:
- Function normally: Most patients
- Be too tight (stenotic)
- Be leaky (regurgitation)
Patients with aortic valve disease may need to have valve surgery if it becomes too tight or leaks too much. Younger patients usually only have features of a leaking rather than a stenotic valve.
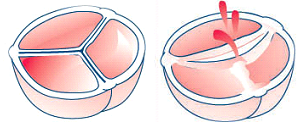
Normal aortic valve Bicuspid aortic valve
The only treatment for BAV (if needed) is surgery. This becomes necessary if leakage (Incompetence) results in symptoms such as congestive heart failure (CHF), angina or syncope (fainting). In asymptomatic patients surgery is indicated if there is evidence of worsening heart function by ECHO.
The decision to repair an aortic valve is made by weighing the risk of repair failure versus the benefit of avoidance of oral anticoagulation therapy.
Most adolescent and young adult patients are concerned about aortic valve surgery because they want to:
- Maintain an active, normal lifestyle, including sports, travel, pregnancy, etc.
- Avoid the use of anticoagulant medications (blood thinners), which some patients are required to take after valve surgery
- Prevent the need for future surgery
A number of factors determine what treatment for aortic valve surgery is optimal:
- Age of the patient
- Expected long-term survival
- Co-existing medical conditions including valve disease, other heart disease or other medical conditions
- Surgery risks
- Risk of thromboembolism (blood clots)
- Risk of endocarditis (infection of a heart valve)
- Valve durability
- Risk of bleeding complications with long-term anticoagulation therapy
- Patient’s lifestyle and personal preferences
Once a decision for surgery is made there are a number of different options available
- Aortic valve repair
- Aortic valve replacement
- Mechanical valve
- Biological valve
- Homograft valve
- Ross procedure (also called the “Switch” operation
Aortic valve repair
Bicuspid aortic valve repair
Advantages:
- Preserved heart muscle strength, and preserved natural heart anatomy
- Decreased risk of infection
- Decreased need for life-long anticoagulant medication
Drawbacks:
- This type of aortic valve surgery is technically difficult.
- Aortic valve repair is only an option for leaky aortic valves, not stenotic valves.
- Although a repaired valve can possibly last a lifetime, some patients may need another valve procedure in the future.
The decision to repair an aortic valve is made by weighing the risk of repair failure versus the benefit of avoidance of oral anticoagulation therapy.
Aortic valve replacement

Mechanical Valve Replacement
Advantages:
- Mechanical valves are very durable and are designed to last a lifetime.
- Re-operations for mechanical failures or tissue in-growth are uncommon.
Drawbacks:
- Due to the artificial material involved, patients who receive a mechanical valve replacement need to take an anticoagulant medication for the rest of their lives. Anticoagulant medications (blood thinners such as warfarin or Coumadin) delay the clotting action of the blood. Anticoagulants help prevent clots from forming on the replaced valve to reduce the risk of a heart attack or stroke.
- Some patients who have a mechanical valve replacement report a valve clicking noise at times. This is the sound of the valve leaflets opening and closing.

Bioprosthetic valve replacement and Homograft Biological Valves
Biological valves (also called tissue valves) are made of tissue, but they may also have some artificial parts to give the valve support and aid placement. Biological valves may be made from cow tissue (bovine), pig tissue (porcine) or pericardial tissue from other species.
Advantages: Most patients who receive a biological valve replacement do not need to take life-long anticoagulant therapy after surgery, unless they have other conditions (such as atrial fibrillation) that require these medications.
Drawbacks: Studies have shown that in a 40-year-old patient, these valves have a 50 percent chance of lasting 15 years or longer, without decline in function. In younger patients, these valves will not last as long, but will still last longer than previous generations of bioprostheses. In older patients they will last longer. The durability of present generation pericardial valves and homografts are very similar.

Homograft (also called allograft) valve replacement
A homograft is an aortic or pulmonic valve that has been removed from a donated human heart, preserved, antibiotic-treated, and frozen under sterile conditions. A homograft may be used to replace a diseased aortic valve, or it may be used to replace the pulmonic valve during the Ross procedure.
Advantages:
- Homografts are ideal valves for aortic valve replacement, especially when the aortic root is diseased or endocarditis (infection) is present.
- Homograft is the best and safest option for patients with severe infections causing aortic valve and root destruction, and abscesses. This is particularly true if the infected valve is a prosthetic valve.
- Homograft valves are well-tolerated by the body because they are most like native valves.
- Most patients who receive a homograft valve replacement do not need to take life-long anticoagulant therapy after surgery, unless they have other conditions (such as atrial fibrillation) that require these medications.
Drawbacks: The availability of homografts can be a drawback. In addition, this type of valve replacement surgery is technically difficult. Homograft valves are expected to last about 15 to 20 years. Like bioprosthetic valves, homografts are not as durable in younger patients.
Ross Procedure (also called Switch Procedure)
The Ross procedure is usually performed on patients younger than ages 40 to 50 who want to avoid taking long-term anticoagulant medications after surgery. During this procedure, the patient’s own pulmonary valve is removed and used to replace the diseased aortic valve. The pulmonary valve is then replaced with a pulmonary homograft.
The Ross operation is not performed when operative findings contraindicate the procedure, or when the pulmonary valve does not appear normal on the echocardiogram, or on inspection during surgery.
Advantages: The pulmonic valve is anatomically very similar to the aortic valve and could be an ideal substitute for the aortic valve. The new aortic autograft is a living valve and it will grow with the patient. The blood flows with less pressure through the pulmonary valve than the aortic valve, therefore a homograft valve could last longer in the right-sided pulmonary valve position. The risk of thromboembolic complications (blood clots, stroke) and the risk of valve infection are very low — lower than for any alternative valve prosthesis. The hemodynamic performance makes the Ross operation an attractive alternative for athletes.
Drawbacks: The Ross procedure is a technically difficult and long surgery, as it requires two valve replacements. Therefore, this procedure is only recommended for young patients who would tolerate a long surgery time. The pulmonary autograft valve is transplanted from the low pressure pulmonary circulation over to the aortic high pressure system. The valve cusps are strong enough to withstand the systemic pressure, but the pulmonary artery wall does dilate when exposed to systemic pressure, occasionally enough to cause the autograft valve to leak.
The risk of requiring re-operation for a leaking autograft valve is about 10 percent within 10 years after the operation.
The Ross procedure is not recommended for patients with tissue defects (such as Marfan syndrome) or for patients who have an abnormal pulmonary valve. The pulmonary homograft in the pulmonary position could also fail; the most common reason for failure is that it becomes stenotic. The risk of requiring replacement of the pulmonary homograft is about 10 percent within 10 years after the procedure.
References:
1) Aortic Valve Surgery in the Young Adult Patient, Gosta Pettersson, MD, Cardiovascular & Thoracic Surgery, Miller Family Heart & Vascular Institute
2) CTSNet Wiki Notes: Aortic valve disease

Comments 1
DAV heart patients can do the gym workouts