LONDON, Dec. 16, 2010: In a press release by Viron Therapeutics about the protective effects of VT-111 during stenting, the CEO of the company announced:
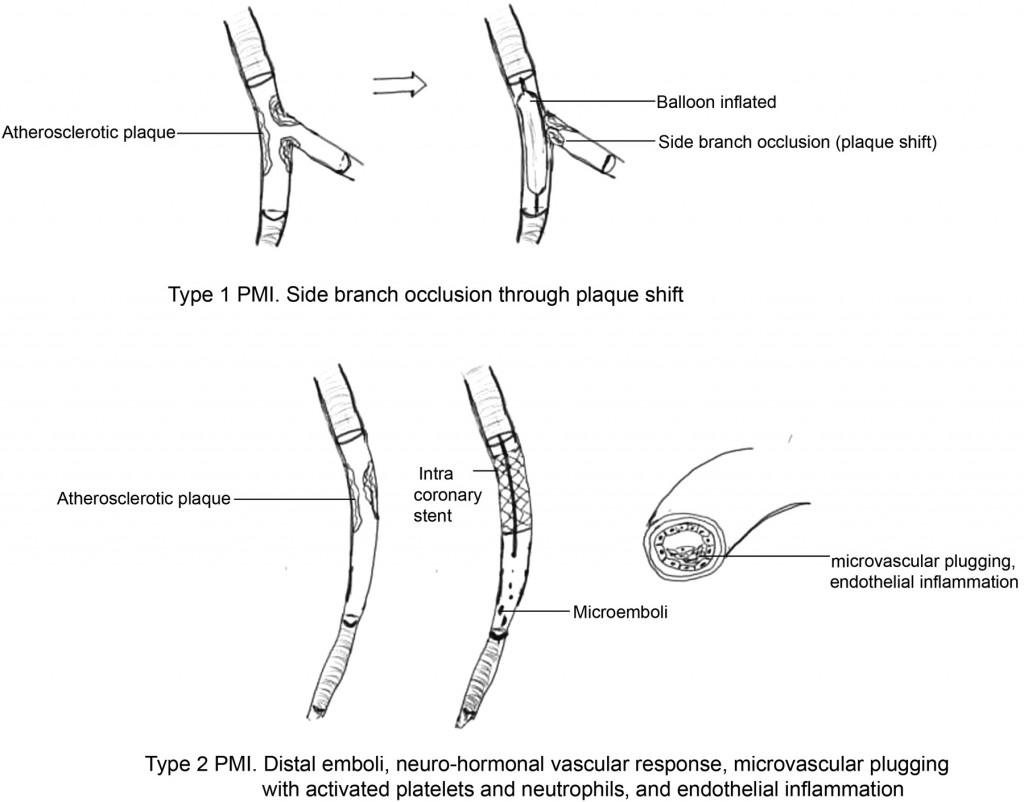
“Although the use of cardiovascular stents have dramatically improved the outcomes for patients with occlusive coronary artery disease, numerous studies have shown that the procedure itself can cause what is termed peri-procedural myocardial injury (PMI),” said James Rae, CEO of Viron. “A recent review in the European Heart Journal shows that 30% of patients receiving coronary stents sustain an injury to the heart tissue arising from the procedure itself and the biomarkers most useful in measuring this cardiac injury are CK-MB and Troponin I.
Viron’s Phase 2a trial showed a statistically significant, dose-dependent reduction in these two key biomarkers of cardiac damage, at multiple timepoints, with a particularly potent effect in the first 24 hours after the placement of the stent. If the incidence of PMI was reduced, clinical outcomes would improve for many of the almost 3 million patients each year that receive cardiac stents in North America and Europe.”
While I don’t question the validity of the study, I do take issue about the statement of dramatic outcome improvement for patients with occlusive coronary artery disease. Overwhelming evidence to the contrary has shown that in patients with coronary artery disease (other than a temporary improvement of angina), stents have no effect on longevity or recurrence/progression of disease except in patients with STEMI.
The additional myocardial damage in 30% of stent patients is cumulative. This means that 1 million patients/year in North America and Europe pay for their stent not only with an increased risk of stent failure (10-15%/year), more stenting (because of initially inadequate revascularization), expensive medications (to protect against disastrous acute stent failure), but also with progressive reduction of function as evidenced by a reduced Ejection Fraction (EF).
If taken into account that in the US, 30% of stent procedures occur in stable CAD patients, who could be treated with equal success with medical therapy alone, this takes on additional meaning, as ultimately survivors will develop heart failure with all the consequences thereof.
Dr T