A subset of patients with diabetes and 3VD was examined in a 2nd paper in 2010.The purpose of this study from Washington State was to examine the application of revascularization strategy in this high-risk patient population of patients with diabestes and multi-vessel coronary artery disease. Specifically, it was sought to determine:
- the revascularization strategies employed in diabetic patients with MVD in Washington State;
- the short-term outcomes of revascularization strategies; and
- the effect of DES introduction has had on the revascularization strategy.
Revascularization trends 1999-2007
PCI for DM trends from 1999-2007
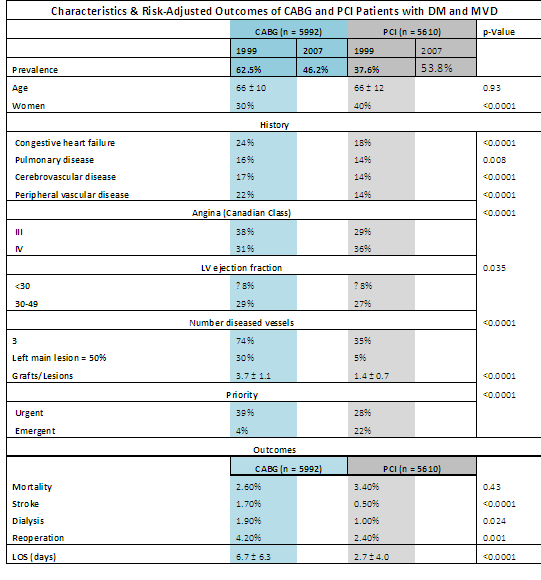
A total of 11,602 Patients with diabetes and 3VD, a sub group of over 150000 patients treated in Washington State from 1999-2007 was compared by treatment with PCI or CABG.During this period, the prevalence of PCI increased from 37.6% in 1999 to 53.8% in 2007, vs. CABG, which decreased from 62.5% to 46.2%. Left ventricular EF was similar between CABG and PCI groups. Seventy-four percent of CABG patients had three-vessel disease, while only 35% of patients treated with PCI had three-vessel disease (p < 0.0001). CABG patients underwent an average of 3.7 grafts per patient, compared to 1.4 lesions treated per patient in those undergoing PCI (p < 0.0001).
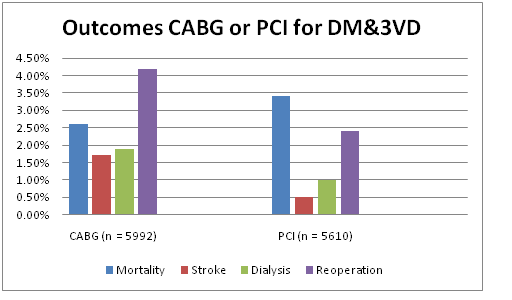
CABG patients had a higher periprocedural stroke (1.7% vs. 0.5%) and dialysis (1.9% vs. 1.0%) rate, longer length of stay (6.7 vs. 2.7 days), higher transfusion rate (45% vs. 7%), and a higher return to operating room (OR) rate (4.2% vs. 2.4%). Short-term mortality was statistically superior for CABG (2.6% vs. 3.4%, p = 0.013).
This study reported on the risk characteristic and outcomes of 11,602 patients with DM and MVD treated over a nine-year period, representing one of the largest series of patients with this profile in the literature.
Most recent studies have consistently shown a benefit of CABG over PCI in patients with MVD and DM. CABG was associated lower major adverse events and low-revascularization rates and associated with lower mortality when compared to Bare Metal ((BMS) or Drug Eluting Stents (DES). These effects were particularly notable when comparing patients with three-vessel CAD and DM. Publication of the SYNTAX trial further corroborated these findings in non diabetic patients with multivessel disease and have not changed with the introduction of DES.
PCI now far exceeds CABG as initial therapy even in patients with DM and MVD. In 2007, the number of patients with DM and MVD in the State of Washington treated with PCI is currently 1.5 the prevalence of those undergoing CABG (722 vs. 492, in 2007), despite both short- and long-term data supporting the superiority of CABG in this patient population. Further, despite all of these patients having at least two-vessel disease, along with an increasing percentage having three-vessel disease in the most recent time period, the number of treated lesions per patient in the PCI group remains well under two.
Since both studies have only described procedural and short term outcomes, it would be interesting to see if follow-up data (when available) indeed confirm trends noticed elsewhere, such as re-intervention and the absence of any survival benefit,
Dr T
(From: Prevalence and Procedural Outcomes of Percutaneous Coronary Intervention and Coronary Artery Bypass Grafting in Patients with Diabetes and Multivessel Coronary Artery Disease, Nahush A. Mokadam M.D. et al, J. Cardiac Surgery, 3 OCT 2010)

Comments 1
Pingback: Physical Activity and Weight Gain Prevention - Cardiac Health