PVCs are an arrhythmia and relatively common. Some people are very sensitive and feel every abnormal heart beat; others are blissfully unaware of them.
Palpitations are feelings that your heart is skipping a beat, fluttering, or beating irregularly, too hard or too fast. Some will be diagnosed by your doctor as Premature Ventricular Contractions (PVCs).
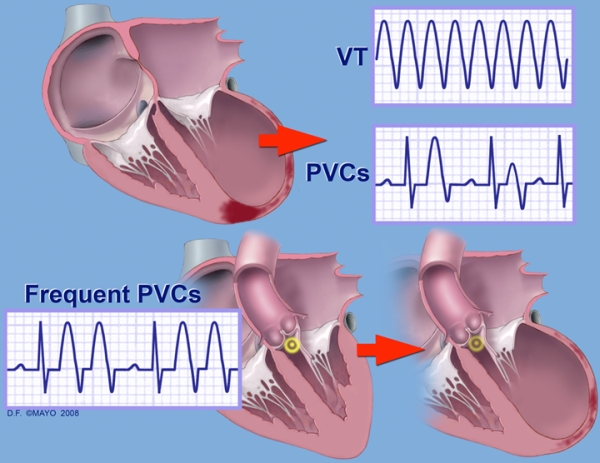
PVCs are extra electrical impulses arising from one of the cardiac ventricles, usually the left ventricle. They are easily detected on an EKG. Sometimes the presence of PVCs indicates an inherent electrical instability in the heart, and therefore indicates an increased risk of sudden death. These “dangerous” PVCs are generally limited to patients with significant underlying heart disease, such as coronary artery disease or valve disease.
More often, PVCs do not indicate any inherent problem with electrical stability, and are completely benign.
PVCs may indicate the presence of underlying heart disease. If a patient has NO significant underlying heart disease, PVCs are probably not dangerous. Most “anti-arrhythmic” drugs are relatively poor at treating PVCs (though they often reduce their frequency.) and can make dangerous arrhythmias more likely. Doctors and patients should thus be very reluctant to treat PVCs with drugs other than Beta blockers (drugs that block the effect of adrenaline). Since Beta-blockers are generally well tolerated and do not make the arrhythmia worse, they are often worth a try. However, patients with NEW palpitations should be checked because that may indicate something serious may have happened to their heart.
In general, patients should try to eliminate caffeine, tobacco and alcohol usage, as it may reduce the frequency of PVCs.
Thus, PVCs sometimes are a marker for underlying cardiac diseases that may be dangerous!
- A variety of underlying cardiac conditions, including coronary artery disease, cardiomyopathy, mitral valve prolapse, etc.
- Abnormal levels of “electrolytes” (minerals) in the blood. Decreased potassium and/or magnesium are the most common associated abnormalities of electrolytes. Both may be caused by the use of diuretics (water pills), among other reasons.
- There are unusual congenital (familial) causes of ventricular arrhythmias.
- Abnormal conditions such as increased thyroid hormones, and others.
- Toxins, including alcohol.
- Stimulants including Caffeine, Nicotine, Cocaine and some over-the-counter medications and herbal/natural formulations contain important stimulants.
- Infection, inflammation or degeneration of the heart muscle.
- Infections at other sites in the body.
- They are often worse with lack of sleep, or stress.
Tests of electrolyte levels, thyroid levels, and other blood tests are frequently done.
An electrocardiogram is necessary to make the diagnosis of PVCs. Since PVCs don’t always occur when one is looking for them, several other means have been developed to assess the frequency and severity of the process in some cases. Holter monitors and event monitors may be useful.
An echocardiogram can assess the function and structure of the heart muscle and it’s valves.
Stress ECHO testing can be completed to assess not only for the possible presence of blockage of the heart arteries (coronary artery disease), but also to see whether more arrhythmias occur with exercise.
Cardiac catheterization, utilizing catheters to measure the pressures in the heart and inject dye in some of its structures, can be very useful in determining the presence of possible associated heart diseases. This is not a routine part of the evaluation, however.
Electrophysiology testing (EPS) can be very informative in some cases. It can be utilized in certain circumstances where the results of the above tests are unrevealing. These studies are performed in the hospital in a suite similar to a heart cauterization lab. Catheters are inserted in veins and/or arteries and advanced to the heart where very precise recordings of the electrical activity can be obtained. In some cases, catheters are also used to stimulate the electrical system to see if abnormal beats can be “induced”.
Beta-blockers (there are many of them) have been shown to cut down both on symptomatic PVC’s in some patients, as well as decrease the risk of sudden death in high-risk patients. In terms of treatment for the palpitations associated with PVC’s, they can often be quite effective but do have side effects that may require their discontinuation.
Specific anti-arrhythmic drugs are designed to cut down on the number of PVC’s by altering the electrical properties of the cardiac muscle. Every “anti”-arrhythmic however, has its own “pro”-arrhythmic properties which have the potential to make the rhythm worse, sometimes dangerously worse. Many trials of medications designed to improve the survival of some types of patients with ventricular arrhythmias actually did the opposite. These drugs have to be used carefully in selected patients who will also need to be monitored closely.
(Image from: Premature Ventricular Contractions and Non-sustained Ventricular Tachycardia: Association with Sudden Cardiac Death, Risk Stratification, and Management Strategies, Indian Pacing , Seth H. Sheldon, MD et al; Electrophysiol. J. 2010;10(8):357-371)


Comments 8
I hear palpitations in my throat
It started when I took soliqua in June
They told me to take it in the morning
15 units . It brought my pulse rate to 39-55 regularily
Then at Dr Appt he noticed fkr first time irregular heartbeat
Never had that before even with sinus tachycardia
Soliqua has side effects of both I mentioned above but he didn’t say to stop it but ordered echo cardiagram 09/30 they haven’t called for my appt yet
I passed areas test 6/13 and ekg was fine
They said I had mild ventricle palpitation which they said not to worry and dr never asked to see me
Tonite the palpitations are in my throat and fast . Afraid to check pulse oxymeter
Mike Risha 980-219-2166
I went walking as usual tonite but ran the last 75 yards , heart hasn’t settled down I guess
I take jardiance at night with bated 81 and pravastatin and losartin
Im 55
I have no chest pain
Or dizziness or heavy legs and arms
When my sinus tachycardia would hit 115 in past my legs felt like jello and heart would race and subside in 20 seconds
Thjs hasn’t happened since may which I thought everything was fine
When my heart rate pulse was up I never had irregular heartbeat
That didn’t happen til pulse was low and using soliqua
It has to be my meds
Is abation surgery recommended for a patient with pvc?
I have had pcv’s off and on for 35 years I’m now 82. My Doc prescribed a beta blocker a few months ago. After taking it for a month the pvc’s started. I hadn’t experienced any for a long time. Stopped the beta blocker but pvc’s continued and they were constant and severe. Late Jan. I went to the emergency room and stayed overnight. There was no heart problem and the cardiologist said not to worry they won’t hurt you. That was good news but I didn’t like the annoying feeling of irregular beats. Stopped drinking coffee and pvc’s stopped in 3 weeks. Didn’t have any for 2 months. Started up again on March 30th and lasted until March 17th when they stopped. I won’t worry about these in the future.
I’ve had PVCs since 2002, caused by extreme stress and also, now, aggravated by second hand cigarette smoke. They usually last about 5-10 seconds.
Yesterday I had am EMG of my neck and shoulders. When I got home, suddenly I had a fairly severe episode that lasted almost a minute. It was scary and I thought I might black out, but then it passed. The electrical shocks obviously triggered this.
Should I get a more thorough test? I was prescribed beta blockers in ’02 that only made the frequency of the PVCs worse.
Thanks for the information. . I came across your site in my relentless quest to find a solution for these darn PVCS. I’m 49 now and started getting them when I was 46. I’ve made two ER trips, the first time they told me it was stress and they were benign after looking at my EKG. I was given a 48 hour Holter Monitor and the results came back normal with PVCS. No other tests were done. They gave me a prescription of Ativan for stress. I took it only a few times. I also started taking 250 mg of magnesium daily and it seemed to help. After a few months they seemed to disappear. I didn’t notice any symptoms for some time.
Fast forward to November of last year and I had another episode that seemed even worse. This time I went to a different ER. They ordered the EKG and this time it showed a partial right bundle branch blockage, but nothing else. Then a 72 hour Holter Monitor. I met with an Electrophysiologist who read me the results and he seemed to laugh it off. He said I was having a few thousand PVCs but they were benign and not to worry about them. MY GP says the same thing. Neither wanted to prescribe any medication other than taking the Ativan if I’m having a panic attack over them. Things cleared up again.
Fast forward to this past week and they’re back again in full force. I think this time they were triggered by a weekend of too much excess drinking. Now I can’t shake them again. It’s been a little over a week and I know I’m getting thousands a day. There is no chest pain, dizziness, etc. but they’re scary as heck. I don’t want to do the ER thing again as I’m sure what they’ll say, not to mention the cost. What can I do to limit the frequency and intensity of these things? I’m probably getting 5 or 6 a minute most of the day. I’ve certainly learned overdoing the alcohol is a no no. But what can I do to hit the reset button again, so to speak? Any idea how long this bad attack will last before I get some relief again?
Thanks for the information I am 74 year old and after 4 o 6 month ago I star feeling something wrong in palpitation I supposed have low back surgery but I afraid even if the doctor said and clear I will waiting to see a specialist in pvc this month
Author
I agree you should have a check up first before any surgery.
Hope this helps,
Dr T