The Coronary Intervention for Persistent Occlusion after Myocardial Infarction (Occluded Artery Trial, (OAT) study evaluated treatment of 2166 high-risk, but otherwise stable survivors of a myocardial infarction and persistent total occlusion of the infarct-related coronary artery.
High risk criteria included an ejection fraction of <50% or proximal occlusion (TIMI flow =0-1). Treatment was randomized to either routine PCI or stenting with Optimal Medical Therapy (OMT) (1082 patients), or OMT alone (1084).
Optimal treatment for patients with acute myocardial infarction with ST-segment elevation (STEMI) includes early reperfusion with primary percutaneous coronary intervention (PCI) or thrombolytic therapy. However, approximately one third of eligible patients do not receive early reperfusion therapy, in many cases because of late presentation.
A patent infarct related artery late after myocardial infarction is associated with better outcomes in comparison with persistent occlusion. Treatment in the US is strongly biased in favor of PCI. Arguments in favor of this include preservation of left ventricular function, increased electrical stability, and the provision of collateral vessels to other coronary beds for protection against future events, weighed against the potential harm from procedure-related complications.
Outcomes
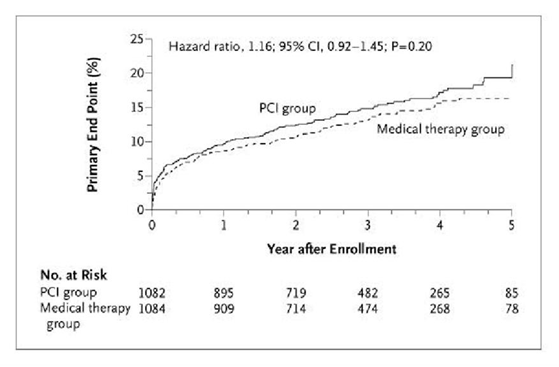
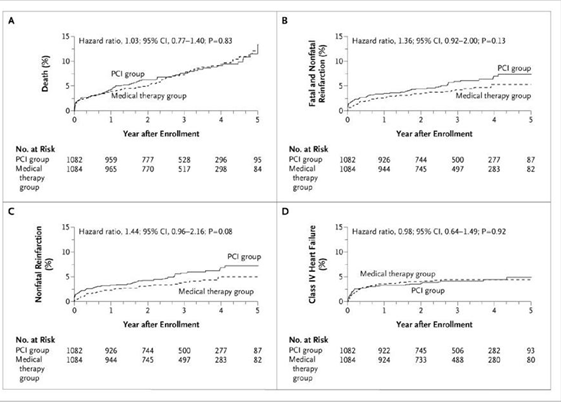
Death from any cause, nonfatal re-infarction, or NYHA class IV heart failure (Primary Outcome):
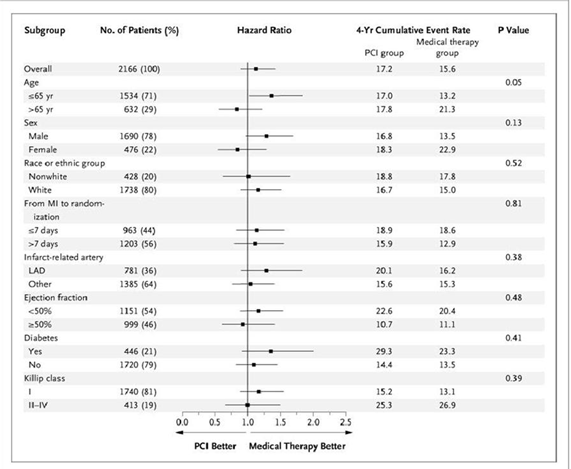
Primary Outcome Sub Groups:
There was no significant difference in the number of confirmed re-infarctions between the PCI group and the medical therapy group, but the rate of site-determined re-infarction tended to be higher in the PCI group (hazard ratio, 1.37; 95% CI, 1.00 to 1.89; P=0.05). There were no significant differences between the groups otherwise. There was a trend toward more frequent coronary revascularization in the medical therapy group than in the PCI group:
There were significantly fewer patients with angina in the PCI group at 4 months and at 1 year. Over time, the occurrence of angina declined in both study groups, as did other differences between the two groups, and by 3 years there was no significant difference between the groups.
Though drug-eluting stents were approved during the later years of recruitment, trials comparing drug-eluting stents and bare-metal stents have shown no reduction with the use of drug-eluting stents. On the contrary, there is growing concern regarding the increased risk of late thrombosis with the use of drug-eluting stents, as compared with bare-metal stents. Moreover, trials of thrombectomy and distal-protection devices to prevent downstream embolization during PCI for myocardial infarction with ST-segment elevation have yielded disappointing results.
Conclusion:
PCI did not reduce the occurrence of death, re-infarction, or heart failure, and there was a trend toward excess re-infarction during 4 years of follow-up in stable patients with occlusion of the infarct-related artery within a month after myocardial infarction.
(From: Coronary Intervention for Persistent Occlusion after Myocardial Infarction, Judith S. Hochman et al. N Engl J Med2006; 355: 2395- 2407)