It has been a while since I have written about improper and unnecessary stenting. Articles in response to a US Senate Finance Committee statement earlier this week have re-activated my concerns about both these activities and the growing industry efforts to influence medical care. The case involves a Maryland hospital, a local cardiologist and a stent manufacturing firm. Other cases against cardiologists in other parts of Maryland as well as in other states are in progress. Charges include stenting in patients without significant coronary artery disease, as well as industry kickbacks.
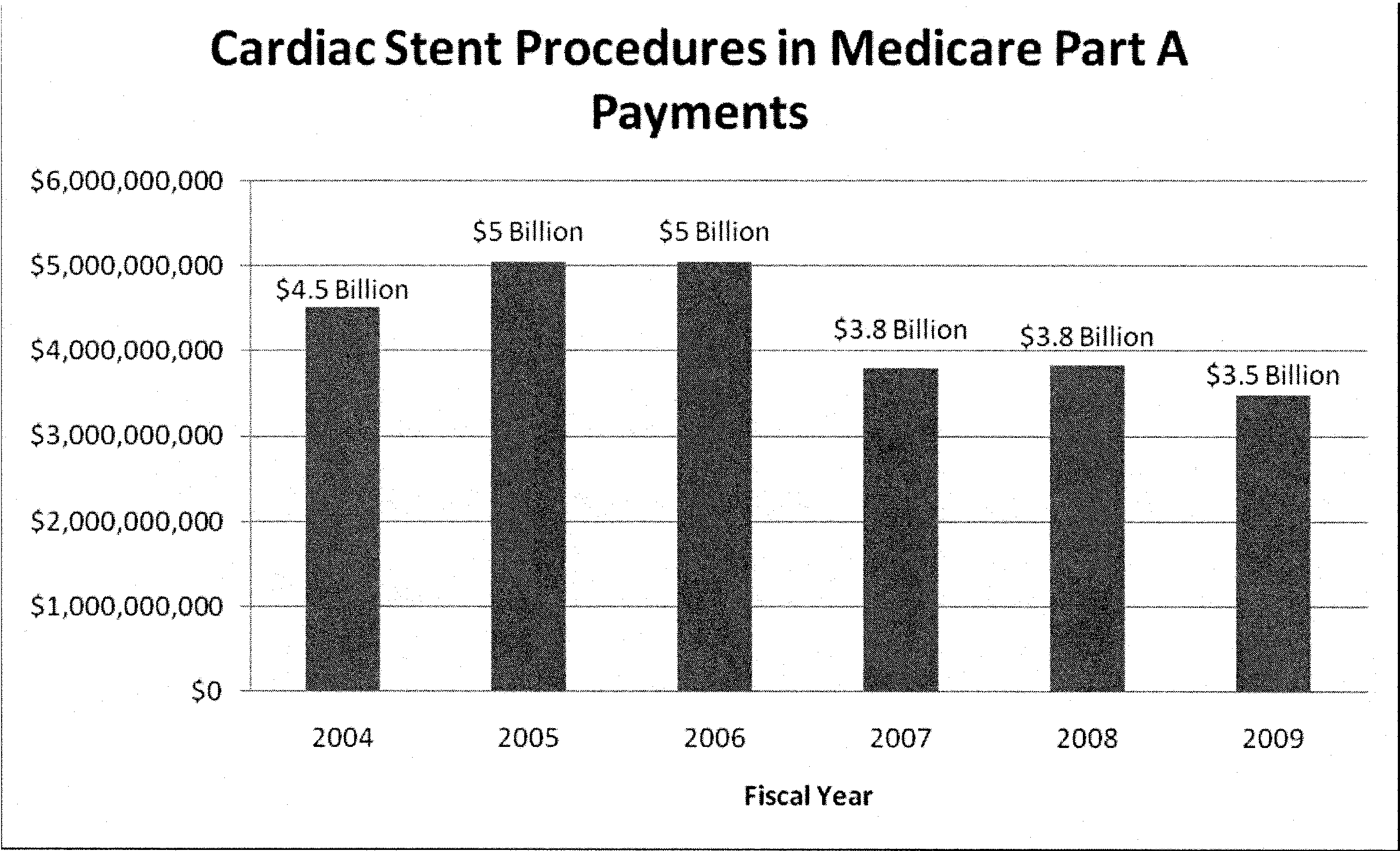
The Senate Finance Committee only reviewed Medicare data, not the overall cost of stenting: From 2004-2009 Medicare alone paid $25.7B for stent procedures in the US, or an average of $5B/year. Approximately 50% of all stent procedures are performed in patients above 65 years of age:
While this report suggests that improper stenting happens in the Medicare population, it does not address its overall occurrence. It also does not review optimal treatment and unnecessary stenting.
Although undoubtedly true that the majority of stent procedures are performed in patients with legitimate coronary artery disease, it has also been demonstrated that of the estimated 1.5 million PCI procedures performed in the US each year, 30% occur in stable CAD patients, who could be treated with equal success with medical therapy alone, at a costs saving of $5 billion of the $15 billion spent on stent procedures each year.
If the number of unnecessary stentswere combined with an as yet unknown number of improper procedures, surely involving more than just Medicare patients, the cost savings would be even more significant, let alone the human cost of medications needed to keep stents patent ($3000) for a year’s treatment and a 10% stent failure rate that will happen whether it was placed for the right indications or not.
Medical device and pharmaceutical industry influence on patient treatments will be the subject of future discussions,
Dr T
Background:
Approximately 17.6 million Americans have coronary artery disease (CAD), at estimated direct and indirect cost in 2010 of $177.1 billion.
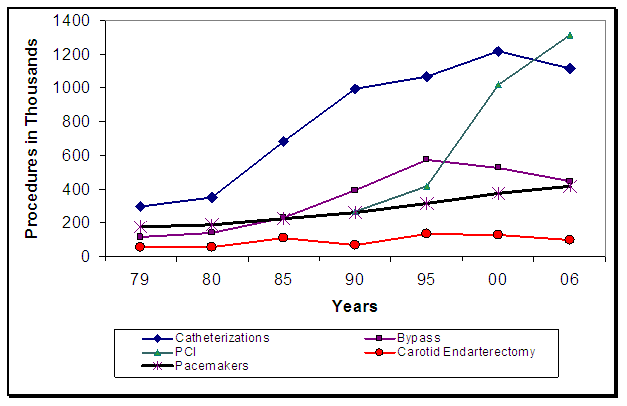
Trends in Cardiovascular Operations and Procedures (United States: 1979-2006). Source: NCHS and NHLBI:
While PCI neither improves survival nor prevents subsequent MI in comparison to OMT, the following recommendations remain valid:
| ACC/AHA recommendations for PCI in patients with chronic stable angina | |
| Recommendations | |
|
|
|
|
|
|
|
|
| Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association; | |
For CABG:
| Guidelines for revascularization with CABG |
|
Abbreviations: ACC/AHA, American College of Cardiology/American Heart Association; CABG, coronary artery bypass surgery; LAD, Left anterior descending; LVEF, left ventricular ejection fraction; SCD, sudden cardiac death; VT, ventricular Tachycardia “Vessel Disease” meaning >50% coronary artery obstruction to flow for PCI & CABG.
http://www.cardiac-risk-assessment.com/patients/news/excessive-stent-use
http://www.cardiac-risk-assessment.com/ca-blog/medical-therapy-for-stable-coronary-artery-disease/