The first three layers of the skin are
- Epidermis
- Dermis
- Subcutaneous tissue
The pH of the skin is approximately 4.5. The slightly acidic pH is due to the acidic protective surface film, which provides some protection against invading micro-organisms.
Epidermis
The epidermis has an average thickness of only about 0.1 mm and it is normally composed of four different layers:
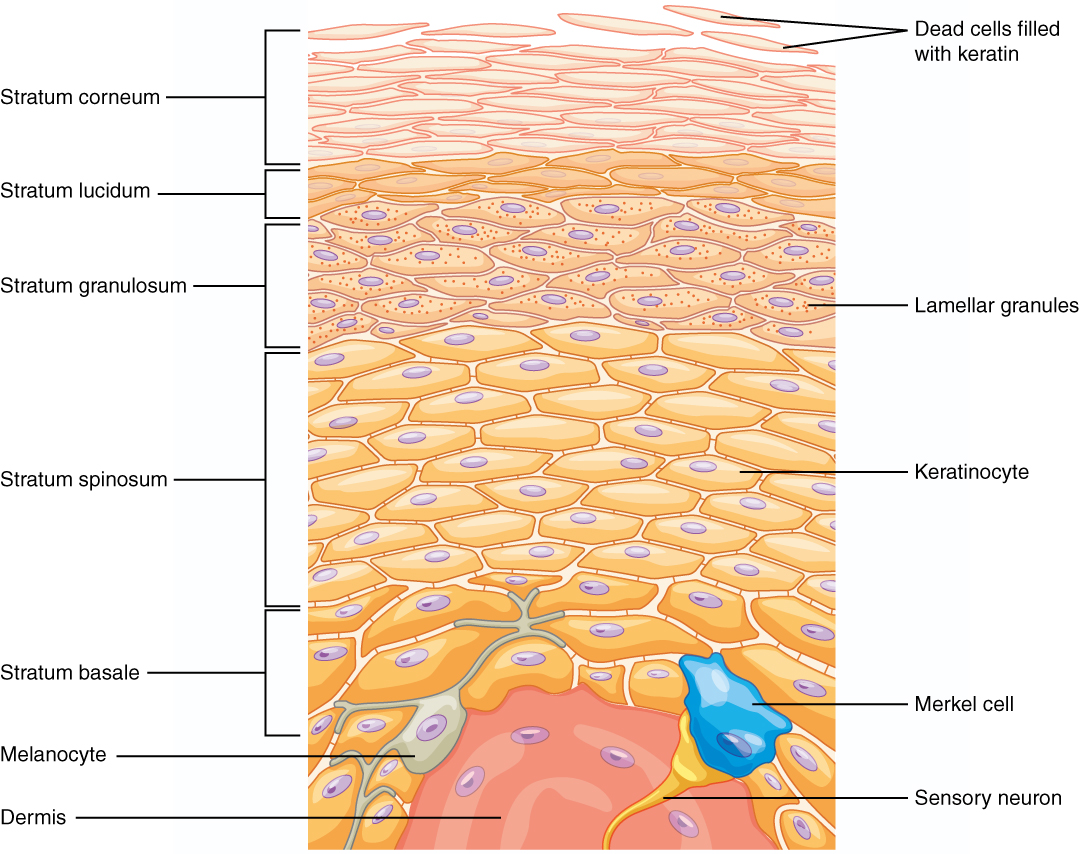
- stratum corneum
- stratum granulosum
- stratum spinosum
- stratum basale.
Where exposure to friction is greatest, such as in the palms of the hands and soles of the feet, the epidermis has five layers. This extra layer is called the clear layer (stratum lucidum), situated between the horny layer and the granular layer.
- The cells of the granular layer synthesise keratohyaline, which is a precursor of the horny substance keratin.
- The prickle-cell and basal layer consist of living cells continually produced through mitotic division. These cells replenish the shed cells of the horny layer and the two layers are referred to jointly, as the germinative layer.
- The other three layers make up the cornification layer. The clear layer, normally found in the thick skin of the palms and soles, is absent in thin skin. It consists of three to five rows of clear, flat, dead cells. The flattened cells become increasingly keratinized as they move through the horny layer and are eventually shed at the skin surface. This process of continual shedding and replacement renews the entire epidermal layer in approximately 27 days.
Dermis
The dermis is the layer that gives the skin its tensile strength and elasticity. These characteristics are derived from the high proportion of loosely interwoven connective tissue fibers (collagen and elastin). Histologically, two layers are distinguished:
- the papillary layer (stratum papillare)
- the reticular layer (stratum reticulare).
The dermis is firmly intermeshed with the epidermis via the connective tissue papillae of the papillary layer. These papillae are interspersed with fine capillary loops, which provide the nutrient supply of the epidermis. The papillary layer also contains numerous free nerve endings branching into the epidermis as well as heat, cold and touch receptors (Meissner’s cells)
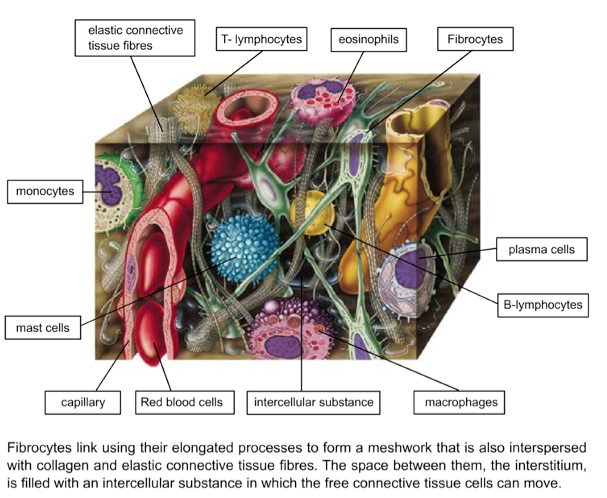
The free connective tissue includes
- fibroblasts,
- macrophages,
- mast cells,
- lymphocytes,
- plasma cells,
- eosinophils and
- monocytes.
Dermal cells and their function:
| Cells | Origin | Function |
| Platelets | Contain clotting proteins (such as fibrinogen, von Willebrand factor & thrombospondin), growth factors (such as IGF-1, PDGF & TGFβ) and chemokines (such as platelet factor 4) | |
| Neutrophils (Polymorphonuclear Leucocytes) | Phagocytosis, particularly bacteria contain Lysosomes containing peroxidase, lysozyme & various hydrolytic enzymes | |
| Macrophage | Ccirculating monocytes | Contain lysozyme & a variety of other hydrolytic enzymes. Secrete Cytokines |
| Fibroblasts | Secrete a non-rigid, extracellular matrix (ECM) that is rich in collagen | Fibroblasts stimulated by Macrophage cytokines migrate to the wound site and secrete ECM. |
| Lymphocytes enable immunity & are specific for a particular antigen | Enable immunity & are specific for a particular antigen | B-lymphocytes secrete antibodies & T-lymphocytes kill virus infected cells & regulate the activities of other white blood cells |
| Plasma B-Cell | Secrete specific antibodies. | |
| Cytotoxic T-Cell | Kill cells that express specific antigens. | |
| Mast Cells | Secrete histamine, a key inflammatory mediator |
The free space, called Extra Cellular Matrix in between, is filled with a gelatinous fluid in which the cells move freely. Mobile fibrocytes link via elongated processes to form a three-dimensional network. They generate components of the intercellular fluid (eg hyaluronic acid) as well as collagen and elastin fibers, which are interspersed within the network of cells. The other free cells of the connective tissue are components of the endogenous defense system and play a major role in inflammation and in the immune regulation of the skin.
- Papillae in the dermal layer are loose connective tissue conical extensions containing capillary blood vessels, free nerve endings and hair follicles extending into the epidermis.
- Meissner’s cells are pressure (touch) receptors found in the dermal layer of the skin.
Section of Loose Connective Tissue of the Dermis:
The reticular layer (stratum reticulare) contains fewer free cells than the papillary layer. The collagen fibers within this layer form a dense network running parallel to the body surface. Between this collagen mesh, the fibers of the elastic connective tissue branch out, giving the skin its extensibility. The direction of maximum extensibility is indicated by Langer’s lines. This is why incisions made perpendicular to these lines cause gaping wounds. In surgical operations, therefore, incisions should be made along these lines wherever possible to improve the cosmetic result. Special modifications of the skin, the hair follicles, sebaceous, sweat and scent glands are embedded in the dermis.
Subcutaneous tissue layer
The dermis merges into the subcutaneous tissue layer without a clear boundary. The loose connective tissue of the subcutaneous layer is interspersed with many of the firm fibers of the dermis, which anchor the skin to the underlying structures, eg the fascia or periosteum. If these retaining bands are few in number the skin moves on its substrate to create a skinfold. For example, on the soles of the feet or the scalp the skin is almost immovable since the fibrous bands are highly developed and numerous.
The entire subcutaneous tissue layer contains pads of fat, which function as either fat stores or structural fatty cushions providing insulation against heat loss, and reducing pressure on underlying structures.
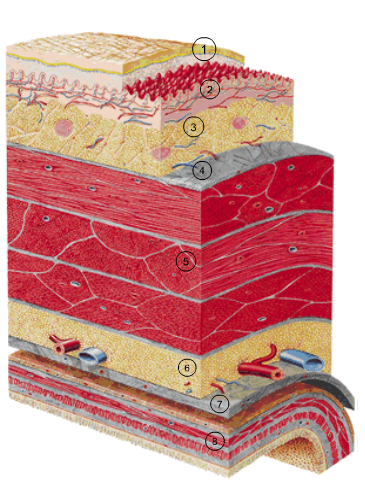
Skin of the abdominal wall with underlying tissue layers
- Epidermis
- Dermis
- Subcutaneous tissue
- Fascia
- Abdominal wall musculature