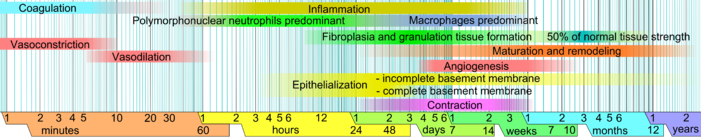
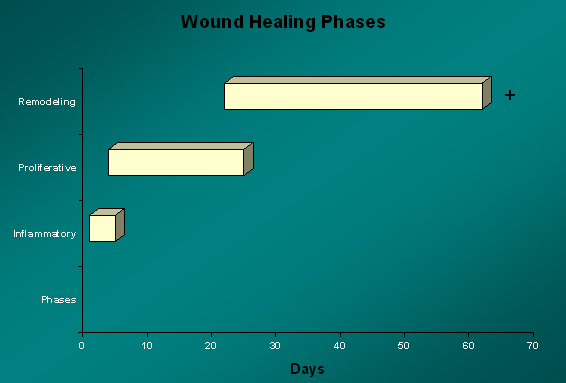
Although wound healing is a dynamic cascade of events initiated by injury and extending well beyond the restoration of tissue continuity, it may be divided into distinct phases, characterized by both the predominant cellular population and cellular function.
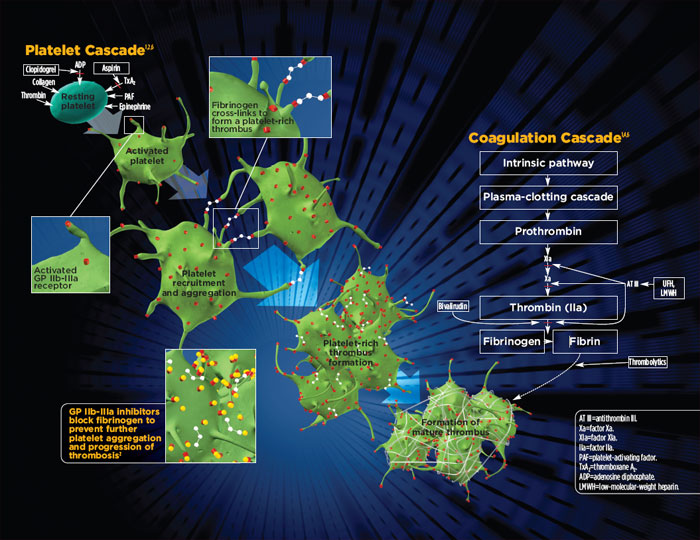
The Coagulation Cascade initiates the first phase of healing. Tissue disruption causes bleeding and contact of platelets with disrupted endothelium causes Platelet Activation, in the form of degranulation and adhesion, leads to hemostasis and chemotaxis of inflammatory cells.
The Inflammatory Phase of healing (injury to 5 days) is defined by neutrophil infiltration with subsequent replacement by macrophages and lymphocytes. Each population of cells acts in response to specific cytokines that are temporally released as the normal healing process progresses. Neutrophils function primarily to clean the wound environment by production of superoxides that kill bacteria and by phagocytosis of necrotic material. Although optimal healing requires that all different populations of cells be present, only macrophages are an absolute necessity.
The Fibroblastic or Proliferative Phase is the second phase of wound healing (days 4 through 12). Macrophages produce growth factors and other cytokines which then promote fibroblast migration, proliferation and collagen synthesis. It is during this phase that tissue continuity is restored; angiogenesis and epithelialization are also achieved.
The Maturation and Remodeling Phase of the scar begins during the fibroblastic phase and is characterized by reorganization of the previously synthesized collagen. Collagen is broken down by matrix metalloproteinases (MMPs) and net collagen in the wound is the result of a balance between collagenolysis and collagen synthesis.
Or: