Although 40-65% of patients admitted for treatment of an acute heart attack with percutaneous coronary intervention (PCI) have multiple blockages, current guidelines strongly suggest to limit the procedure to the blocked artery (the culprit vessel).
PCI in “Non-culprit coronary arteries” is associated with a significantly increased risk of dying, as Armstrong and colleagues of the APEX-AMI trial recently published in the European Heart Journal of June, 2010.
The investigators analyzed data from the earlier APEX-AMI trial, which took place in several centers around the world. Among the 5373 patients who underwent primary PCI, 2201 (41%) had multi-vessel coronary artery disease.
Patients with single-vessel disease only underwent culprit-artery PCI, and had a lower 90-day mortality than patients with multi-vessel disease (3.1% vs. 6.3%, p<0.001).
Of the patients with multi-vessel disease, most (>90%) just underwent PCI to the culprit vessel, but in 10% of cases other diseased coronary arteries were also stented. As the curves suggest, adverse outcomes became only apparent well after discharge following the intervention:

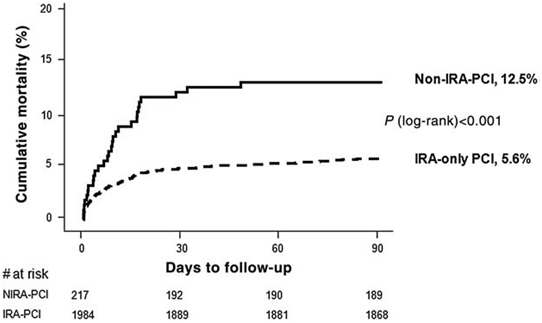
Kaplan–Meier curve of 90-day mortality in patients with non-IRA PCI vs. IRA-only PCI. (IRA=Infarct related Artery)
Despite this, non-culprit coronary interventions were performed concurrent with primary PCI in 10% treated at experienced and high-volume PCI centers in North Americas and Western Europe at more than twice the risk (OR=>2.3, p=0.001 ):

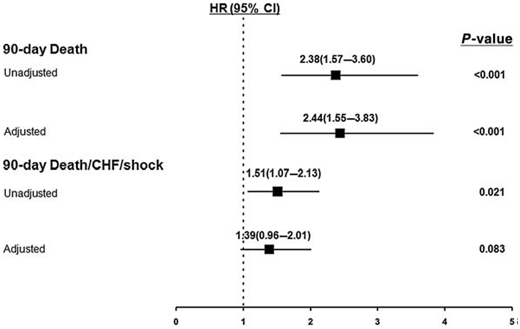
Unadjusted and adjusted hazard ratios of 90-day mortality and 90-day death/CHF/shock (post-first-balloon-inflation) in patients with non-IRA PCI vs. IRA-only PCI.
Geographic variations were probably related to the “more ‘aggressive’ interventional environment where fee for services and procedures may influence behaviors” in Western countries.
Comments:
As is so often the case, more is not always better, although a question remains why higher mortality rates only became visible after a period of time. Nonetheless, there was no evidence that more interventions improved survival, and certainly economic rewards should not play a role in clinical decision making.
This suggests perhaps that other factors, such as patient characteristics played a role as well, or is it because multiple interventions also multiply the risk of PCI failure?
Dr T
Referemce:

Comments 2
Interesting article–I’ll have to take a look. Do you have any more thoughts on why interventions on multiple vessels have increased mortality? Is it that these people are more likely to die from MI within the 90 days?
Love to hear your thoughts, and thanks for this blog!
Dear Dr. Smith,
Most of the patients with multivessel disease had PCI only in the lesioned artery (90.1%), while 217 (9.9%) received additional PCI in a non-culprit coronary artery. Non-culprit artery PCI was more common in North America (12.6%) and Western Europe (10.5%) than in Eastern Europe (6.6%) and Australia/New Zealand (6.1%) (p=0.001).
This particular article did not address cause, only effect.
I speculated that other factors, such as patient characteristics may play a role or because multiple interventions also multiply the risk of PCI failure.
Dr T