Acute Stent Thrombosis frequently results in myocardial infarction (up to 80% of cases) with reported mortality rates between 30 and 45%.
In contrast, Coronary Artery Bypass Graft occlusion may become apparent with recurrent angina, which then may lead to repeat revascularization. This effect is well known from the literature and did indeed translate into increased rates of myocardial infarction and cardiac death in the SYNTAX trial.
“CABG remains the standard of care for patients with three-vessel or left main coronary artery disease”(2)
While stenting is of course not responsible for the Atherosclerosis, it causes severe local damage to the artery involved; the result an inflammatory reaction that involves the area that is stented as well as a zone up – and down stream of the artery, thus the 10-15% yearly failure rate/stent.
In essence a stent produces a new disease and to prevent the built-in complications, all those drugs are given to suppress the inflammatory response. An acute event is usually the result of plaque hemorrhage with acute occlusion of the artery involved, which is what probably happened. He died before an examination of the heart would have shown actual necrosis.
There are many articles (and I have reported on them many times) showing stents do not protect against future heart attacks or prolong life, as opposed to bypass surgery (CABG), which has much superior results in patients with 3-vessel CAD such as your father.
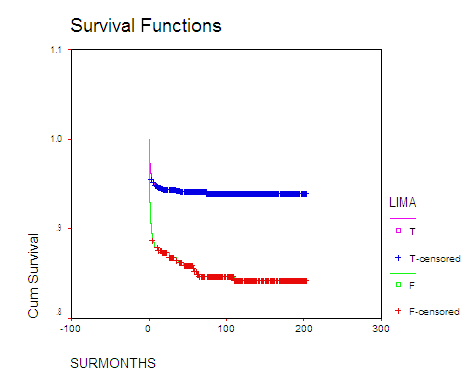
In contrast, if your father had been treated with bypass surgery (CABG), I am 99% certain he would be alive today (accounting for a <1% operative risk in a healthy male patient with normal heart function – similar to the risk of stenting).The following Kaplan Meier survival analysis was done on my patients during the period 1986-2001 with almost 200 months follow-up:
The upper curve shows the long term (193 months) survival in CABG using a Left Internal Mamary Graft (LIMA): 94%, the operation your father would have had. The lower survival curve reflects an 86% long term survival, including all other cardiac operations.
Although the literature has associated CABG with a higher risk of stroke than PCI, this was not at all the experience in my practice.
Even so, almost all literature confirms my opinion of a superior outcome with CABG, especially in patients with 3-vessel disease, diabetes and or diminishe heart function.
An important issue in the therapy for multivessel or left main CAD is that of re-intervention due to stent restenosis or graft occlusion. Although failure rates of the initial revascularization procedure were found to be not significantly different for PCI and CABG in the SYNTAX trial, the consequences of the two respective events are known to differ enormously.
In summary:
Patients with extensive (“3 vessel”) disease that may include a “Left main stenosis”, diminished heart function and/or diabetes do much better with a bypass operation. In situations where time is of the essence, such as an acute heart attack, a stent may the best option if treatment is quickly enough (w/i 8 hrs of the event). The same is probably also true for patients with only “one or two” vessel disease, although there are mini bypass operations that offer an equal if not superior treatment because it promises a much better long term protection.
1. Best way to revascularize patients with main stem and three-vessel lesions. Patients should be operated! H. Reichenspurner et al, Clin Res Cardiol 2010 Jul 9
2. “CABG remains the standard of care for patients with three-vessel or left main coronary artery disease” (Serruys et al. in N Engl J Med 360:961-972, 2009).
3. Pathology of acute and chronic coronary stenting in humans. – Farb A – Circulation – 5-JAN-1999; 99(1): 44-52