I thought to post a recent evaluation of a patient who contacted me for consultation:
Mrs. XYZ, DOB: 1955
57 years old White Female, with low level Angina and progressive loss of exercise tolerance (fatigue, “can’t do much anymore”).
(A significant factor in her care may well have included no health insurance, even though she rendered full payments at the time of her treatments).
Past Medical History:
This patient was admitted to a local hospital in December, 2005 with acute chest pains. Upon admission, an old AMI was noted on EKG, but a new infarct was excluded. Because of unstable symptoms, she underwent urgent cardiac catherization, showing 2 Vessel CAD (100% LAD, 50% Ramus Intermedius, mild non-obstructive disease RCA), with apical and anterior LV akinesis, Heart function moderate dysfunction (LVEF=40%, LVEDP=15 mmHG).
Her symptoms stabilized and a decision was made to treat her medically with an F/U Office Visit scheduled 6 months later.
Review of available data from the only follow-up office visit, D.D. 12/27/2005
Chief Complaint:
- Low level angina;
- Minimal exercise tolerance;
- SOB with moderate exercise, not at rest, none at rest or when laying flat;
- No swollen legs;
- No palpitations or dizziness.
Past Medical History:
Admitted to Hospital on 12/9/2005 with chest pain (Myocardial Infarction apparently excluded). Because of unstable symptoms, this patient underwent urgent cardiac cath. showing the following:
- 2-vessel Coronary Artery Disease with proximal Left Anterior Descending CA (LAD)100% occluded, filling late via Left sided collaterals, 50% Ramus Intermedius Circumflex CA, Right CA mild (<50%)diffuse disease;
- Left Ventricle: Ant +Apical wall akinesis, EF 40%, LVEDP: 15 mmHg.
Exam in follow-up on 12/27/2005:
WNL, VSS, BP: 102/72, pulse 78 BPM, Lungs clear
Impression on 12/27/2005:
- S/P old Anterior Myocardial Infarction,
- Ischemic cardiomyopathy
- Hyperlipidemia (no data available)
Treatment: (Appropriate therapy in my opinion for this patient at that time)
- Metoprolol 25 mg BID
- Benicar, (?) HCTZ
- Vytorin
- Low salt diet
Office Visit 5/24/2006:
Recurrent symptoms with Angina Pectoris up to twice daily; no other complaints or findings.
Exam: unchanged from previous visit
Rx:
- Isordil 20 mg BID
- Consider repeat Cardiac Catherization if no improvement
On the only follow-up visit since 2006 the patient was advised that nothing could be done, and asked only whether she was afraid to die.
Risk Factors:
- Female gender
- Smoking
- Moderate obesity
- Hyperlipidemia
Review Of Systems: Negative
Exam:
- White Female, No acute distress
- Height: 5.2 Ft (157 cm)
- Weigh: 140 lb (66 Kg)
- BMI: 27
- Blood Pressure: 105/75
- Pulse: 75 BMP
- Resp. Rate: 12
- No evidence of vascular disease, pulses etc. intact;
- Otherwise exam benign, moderate central obesity, heart/lungs ok, abdomen benign, pulses intact, no murmurs or bruits. No peripheral edema.
Discussion:
- 57 years old White Female with low level angina, 2 V CAD, moderately impaired LV (heart function EF= 40%)
- Moderate central obesity
- Hyperlipidemia
- Continued smoking
- No re-evaluation since 5/24/2006.
Recommendations:
- The recurrent and present symptoms suggest ongoing ischemia and continued myocardium at risk. A Stress ECHO followed by a repeat cardiac catherization should be considered ASAP, as it is likely that progression of disease has occurred in the interval since 2006. A CT Coronary Angiogram is not indicated since the patient has known Coronary Artery Disease;
- As the 100% occluded LAD lesion is most likely not amenable for a PCI (angioplasty), this patient should be considered for elective/urgent (depending on the findings) Coronary Artery Bypass Grafting (CABG) *3 to LAD, Ramus and probably RCA (my anticipated result from a catherization);
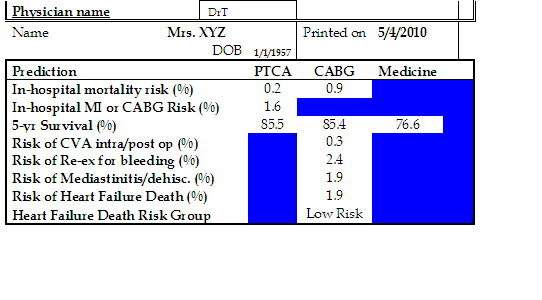
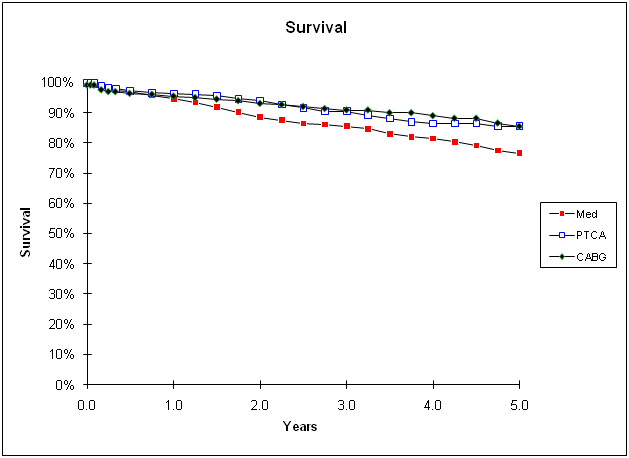
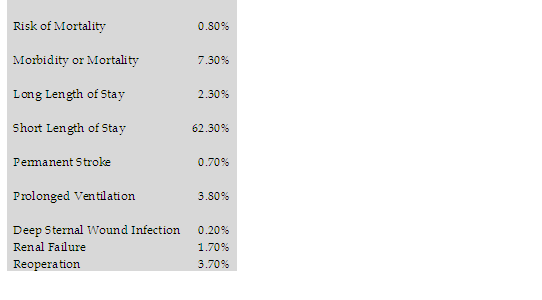
- The risk of this operation is less than 1% (based on personal experience, Euroscore, STS and NNECVSG Risk analyses):
STS Risk analysis algorithm:
NNECVSG Risk algorithm:
I wanted to show this case because it highlights a number of issues:
- Is there information that was not passed on to the patient, but that precluded further treatment?
- Did her lack of insurance influence her doctor’s recommendation?
- When this patient was told nothing could be done, she accepted this verdict until she contacted me via this website. It is not uncommon for patients to blindly follow instructions even though (as happened here) this means a certain death sentence;
- It is vital that patients look for more information or ask for a second opinion when they are unsure that they receive optimal treatment for their condition.
Situations such as what occurred with Mrs XYZ are less uncommon than one would expect. I used her case to demonstrate what an evaluation and consideration of all options includes. The calculations were used to confirm my own observations, but did not alter my opinion.
Please tell me what you think,
Dr T


Comments 1
Hi Dr. T–
Wow–what a consultation! I’d send a patient to you anytime.
I wonder if reading between the lines the MDs involved felt the patient would be a poor candidate for any kind of intervention? or the patient maybe hadn’t followed through with recommendations/appointments (I mean no disrespect to the patient involved)? The plan had been after all to do a cath if the patient wasn’t better.
I certainly agree however that if the patient has any question of unstable angina further work-up is needed ASAP. Also, it is clear there is at the least a clear lack of effective communication between the doctor and patient, the latter who clearly feels abandoned (recalls only that she was asked if she was afraid to die). A second opinion is always a good idea, even if just to reassure the patient that her treatment plan is probably the best one for her.
Thanks for this great blog.
Jane