POTS is a condition in which a change from supine to an upright position causes an abnormally large increase in heart rate, called tachycardia.
Studies have shown a decrease in blood flow to the brain when that occurs. Patients with POTS may have problems when changing position, even when moving from one chair to another or reaching above their heads. Many patients also experience symptoms when stationary or while lying down. POTS can be severely debilitating and some patients are unable to attend school or work, and severe cases can completely incapacitate the patient. Most patients will respond to some form of treatment. Lifestyle changes, particularly drinking extra water and avoiding trigger situations such as standing still or getting hot, are necessary for all patients. Some patients also benefit from the addition of other treatments, such as certain medications.
When the body cannot effectively adjust to upright posture, a person is said to have orthostatic intolerance. POTS is defined by excessive heart rate increments upon upright posture and includes symptoms of orthostatic intolerance associated with an increase in heart rate from the supine to upright position of more than 30 beats per minute or to a heart rate greater than 120 beats per minute within 10 minutes of head-up tilt.
There is more to POTS than just a rising heart rate with change of position. It also requires a drop in blood pressure (together called “Orthostatic symptoms”), and is often associated with a lot of other symptoms.
In people with POTS, the “autonomic system” seems to be out of balance and blood is not going to the right place at the right time to do what the body needs. To make the diagnosis, a host of other illnesses need to be excluded that include thyroid disease, cardiac disease, medication side effects and anxiety disorders, to name as few.
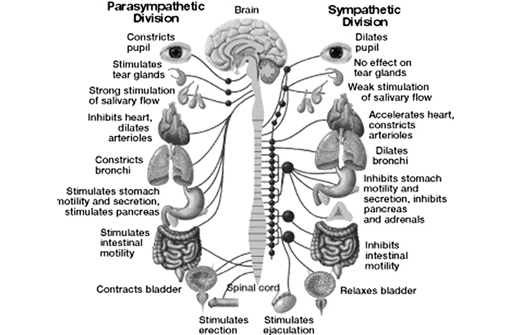
The Autonomic System
The autonomic nervous system is responsible for regulating a multitude of organs and functions throughout the body. Some of these functions include temperature, respiration, heart rate, blood pressure and the digestive tract. A patient experiencing ANS dysregulation may experience abnormalities in the many organs and functions the ANS regulates.
The symptoms of postural orthostatic tachycardia often mimic other illnesses. Entities such as thyroid disease, pheochromocytoma, hypoadrenalism, cardiac disease, autonomic neuropathies, medication side effects and anxiety disorders need to be ruled out before a patient is labeled with POTS.
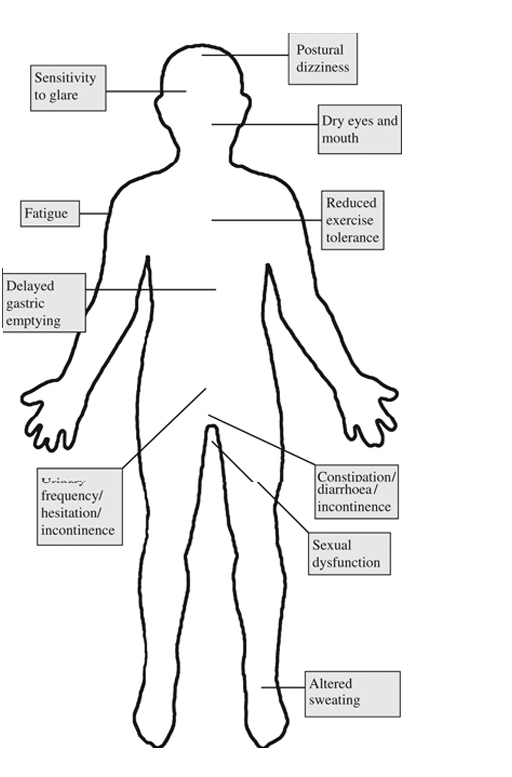
Symptoms that may be associated with Autonomic Dysfunction
There are a variety of tests that the POTS patient may undergo. Orthostatic symptoms are usually the most debilitating aspect of autonomic dysfunction. and for this reason the blood pressure and heart rate response to upright posture should be the starting point of any evaluation.
A Patient may be given various tests to determine how dysautonomia is affecting their heart. Sinus tachycardia commonly occurs in those with POTS. A patient may be asked to wear a Holter monitor to determine if their heart is functioning correctly. Irregular heart rhythms are recorded and then evaluated by a physician.
A stress test can be used to determine how exercise might affect the POTS patient. Sometimes an echocardiogram will be performed along with the stress test. This test helps physicians identify abnormalities in the heart’s structure and function.
One of the most commonly used techniques for assumption of orthostatic stress is head-upright tilt table testing (TTT). This testing requires specialized equipment, (i.e., a tilt table) and trained technician/physical therapists for proper administration.
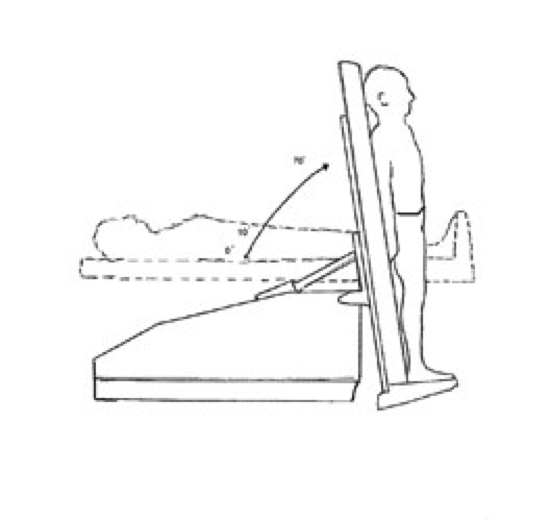

 The most common TTT protocol is one that incorporates an angle of upright tilt of 60-80°, which is generally sustained for 30-60 minutes or until signs and/or symptoms of orthostatic intolerance ensue. The immediate cardiovascular responses to TTT in a healthy population is an increase in heart rate (HR), slight fall in systolic blood pressure (SBP), slight increase in diastolic (DBP) and maintained mean arterial blood pressure (MAP).
The most common TTT protocol is one that incorporates an angle of upright tilt of 60-80°, which is generally sustained for 30-60 minutes or until signs and/or symptoms of orthostatic intolerance ensue. The immediate cardiovascular responses to TTT in a healthy population is an increase in heart rate (HR), slight fall in systolic blood pressure (SBP), slight increase in diastolic (DBP) and maintained mean arterial blood pressure (MAP).
These cardiovascular responses are attained through adequate and appropriate autonomic response to the orthostatic challenge. Alterations in the response of one or both branches of the autonomic nervous system may compromise the cardiovascular response to TTT, which can be defined by measuring the HR and BP response during an orthostatic challenge.
Orthostatic hypotension in POTS is defined according to the American Autonomic Society and American Academy of Neurology as a decrease in SBP of ≥20mmHg and/or in DBP of ≥10mmHg.
Therapies for POTS are targeted at relieving low blood volume or regulating circulatory problems that could be causing the disorder. No single treatment has been found to be effective for all. Some treatments are more successful than others and are often used together for best results. Simple interventions such as adding extra salt to the diet, and avoiding heavy meals and alcohol are often effective. Some people with POTS avoid faintness by sleeping with the head of the bed tilted up or by using a body stocking. The drugs fludrocortisone (for those on a high salt diet) and midodrine in low doses are often used to increase blood volume and narrow blood vessels. Drinking 16 ounces of water (2 glassfuls) before getting up can also help raise blood pressure. Some individuals are helped by beta-receptor blocking agents. There is some evidence that an exercise program can gradually improve orthostatic tolerance.
POTS may follow a relapsing-remitting course, in which symptoms come and go, for years. In most cases (approximately 80 percent), an individual with POTS improves and becomes functional, although some residual symptoms are common.



Comments 1
I have pots do 3 yrs ago. I work as a recovery rm nurse on my feet all day with one 30 min break with call. I got sob couldn’t climb stairs then just sleeping my heart would beat so fast I literally could feel it before finally getting a correct diagnosis tilt table. I have had chronic constipation contributed to a lot of intestines. Ok🙄