In the SYNTAX trial 1800 patients with previously untreated left-main or three-vessel disease were randomized to CABG or PCI.
As expected, differences in long-term outcomes of Coronary Artery Bypass Grafting vs. PCI, already present after year one, have continued to become more obvious during the next four years:
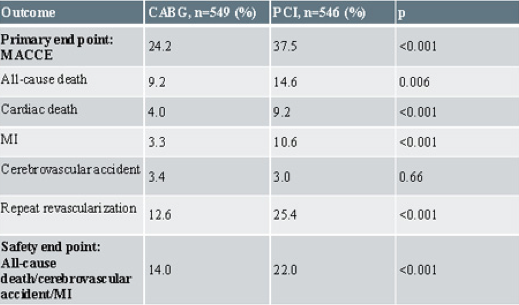
SYNTAX five-year results for patients with three-vessel disease:
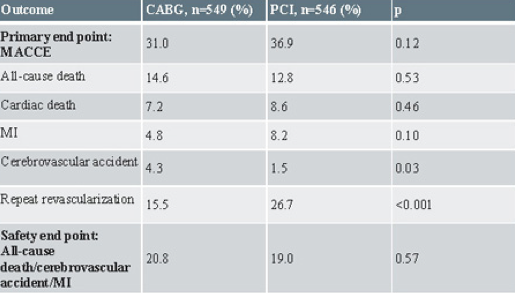
SYNTAX five-year results for patients with left main disease:
- After five years patients who underwent Coronary Artery Bypass Grafting continued to have better outcomes than with PCI. This was especially evident in patients with three-vessel disease.
- Patients with left main disease and less than three vessels involved had equivalent rates of major adverse cardiac and cerebrovascular events (MACCE).
- In 3VD patients CABG outcomes were superior to PCI (p<0.001).
- After four years CABG vs. PCI stroke rates equalized in 3VD.
- In the PCI group almost five stents/patient were used for a total length of about 9 cm. Despite this, only a little over 50% were completely revascularized.
- In the CABG group, about three grafts/patient were placed for a revascularization of 63.2%, only marginally better than in the PCI.
- Despite this, during the five-year follow-up PCI patients underwent repeat revascularization at more than double the rate in 3VD (12.6 vs. 25.4; p<0.001), LMD (15.5 vs. 27.7; p<0.001).
Summary and conclusion through the previous four years
- At 1 year, the incidence of the primary composite endpoint MACCE (death, stroke, myocardial infarction, or repeat revascularization) was significantly lower with CABG than with PCI (17.8%, vs. 12.4% for CABG; P=0.002).
- After two years CABG showed superior outcomes with the PCI cohort showing an increased incidence of MI.
- At three years, only the group with the lowest SYNTAX score had equivalent outcomes. The intermediate and high-risk groups clearly showed a survival benefit if CABG was performed.
- Four-year results suggest that CABG remains the standard of care for patients with complex lesions (intermediate or high SYNTAX Score). With less complex disease (low SYNTAX Scores), PCI is an acceptable revascularization alternative.
Characteristics of the SYNTAX Patients
|
Patient Characteristics |
|
|
PCI |
|
|
n=903 |
|
| Age |
65.2 ± 9.7 |
| Logistic EuroSCORE |
3.8 ± 4.5 |
| Parsonnet score |
8.5 ± 7.0 |
| SYNTAX Score |
28.4 ± 11.5 |
| Number of lesions treated |
3.6 ± 1.6 |
| Number of stents used |
4.6 ± 2.3 |
| Total length stented |
86.1 ± 47.9 |
| Complete revascularization |
56.70% |
|
CABG |
|
|
n=897 |
|
| Age |
65 ± 9.8 |
| Logistic EuroSCORE |
3.9 ± 4.4 |
| Parsonnet score |
8.4 ± 6.8 |
| SYNTAX Score |
29.1 ± 10.0 |
| Number of Grafts |
2.8 ± 0.7 |
| Complete arterial revascularization |
18.90% |
| Off-Pump surgery |
15% |
| Complete revascularization |
63.20% |
In addition, 816 patients (41%) could not be randomized and were assigned to another registry:
- 6% of patients were only treated with PCI, due to severe co-morbidities
- 35% of patients were only treated with CABG, due to complex anatomy judged unsuitable for PCI
- In patients not eligible for PCI, surgery provided excellent long-term results.
|
Reasons for Registry Allocation |
|
|
PCI Registry |
|
| High Surgical Risk |
71% |
| No graft material |
9% |
| Patient refused CABG |
6% |
| Patient refused CABG |
6% |
|
CABG Registry |
|
| Complex Anatomy |
71% |
| Untreatable CTO |
22% |
| Unable to take Anti-platelet Rx |
1% |
| Patient refused PCI |
1% |
| Other |
6% |